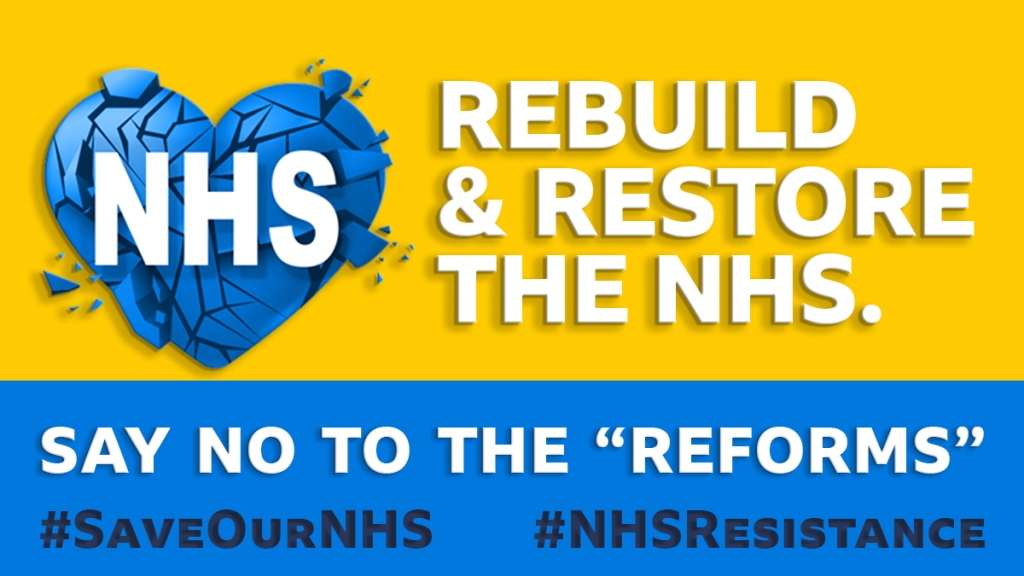
We can see the damage to our health care. What can we do about it?
We can
- Understand what is happening. Check any information carefully as sections of the press are untrustworthy. Record our own experiences
- Talk to other people. The value of one-to-one conversations with trusted friends cannot be underestimated. Such talk is the basis of all campaigns.
- Know what we want for the health service instead of today’s chaos. We want the NHS without privatisation, fully staffed, fully funded with decent wages and working conditions. We do not want private companies, we do not want CIPs and closures, not long multi-million waiting lists or denial of treatment.
- Organise to restore the NHS. How do we do this?

Conversations.
Organising together with other local or workplace campaigners producing and distributing leaflets, social media, meetings, demonstrations, pressure on politicians, industrial action, and popular education. We know what campaigns look like. We know such campaigns take work and effort but nothing worthwhile was ever won without one.
Shout out to the Suffragettes, the Tolpuddle martyrs, Equal Pay, the
Hillsborough Justice Campaign, the Abortion Rights Campaign, Equal Pay Campaign, the Shrewsbury parents, the Covid Bereaved Families, Anti-Apartheid, the Right to Food and Fans supporting Foodbanks and all the trade unions
They all fought and are still fighting long and loud. Sadly, that is what we must do now.
We know the health privatisation lobby funds politicians in all parties but some Conservatives have even written books about how the NHS should be privatised. They cannot deny it. Others are more shamefaced and should be shamed some more.
75 years ago a war-wrecked country started the NHS. It is time to win it back!
Restore and Repair the NHS on its 75th Anniversary!
75 years ago, the post-war government founded the NHS. For the first time every person, rich or poor, had access to world-class healthcare, free at the point of need. The government had responsibility for the health care of the entire population. The NHS helped the people and the whole country recover from the war and helped its children to grow up well and strong.
“It will provide you with all medical, dental and nursing care. Everyone – rich or poor, man, woman or child-can use it or any part of it. There are no charges, except for a few special items. There are no insurance qualifications. But it is not a “charity”. You are all paying for it, mainly as taxpayers, and it will relieve your money worries in time of illness.”

Who fought to set up the NHS? It was ordinary people. there were campaigns for healthcare through the early twentieth century. It was not given to us by the rich and powerful. Who fought for the NHS to be founded? Trade Unions, working-class Women, Socialists, The Socialist Medical Association, returning armed forces, and the Labour Party.

Let us go back to that tradition and once again fight for our NHS. Talk to your friends, family and workmates about this.
Who opposed the founding of the NHS? The Conservatives. 75 years later they are wrecking the NHS
We deserve better. We have the right to world-class speedy treatment and this government is taking it from us.
Greedy Conservative ministers say the economy cannot afford the NHS. On the contrary if the NHS crashes, the economy suffers. A poorer health system means lower life expectancy over time (and that is happening in the US) and more sickness in the workforce. That means fewer people are able to produce value and the productivity of those able workers not rising much. So, it means an economic slowdown.
How did the NHS develop once it was founded?
The NHS worked like this; the government was responsible in law for providing healthcare for its citizens.
- Healthcare was a national, publicly provided system.
- The NHS was for everyone, rich or poor young or old, citizen or visitor.
- All treatment was free at the point of need.
- The best available treatment was available to all.
- Staff were reasonably well paid and qualified.
- The NHS was a research institution so treatments could be evaluated.
- The NHS was the world’s largest purchaser of drugs so could negotiate with the drug companies for better prices and safer drugs.
Everyone paid taxes and the Government funded healthcare and the NHS grew. Right from the start there were sniping attacks on the NHS but it was so popular politicians did not dare attack it openly. Bevan the founder of the NHS resigned as the Minister when prescription charges were introduced.
It remained, despite cuts, the best health service in the world until 2017, largely living on earlier investments. Then cuts and privatisation ramped up.

Privatisation began under Thatcher who privatised hospital cleaning, which lead to hospital-acquired infections like MRSA.

Her cabinet discussed full-scale privatisation, including bringing in health insurance to make people in work pay but did not dare implement it. She also started the privatisation of much of our elder care. Most care homes are now owned by big companies. Then Tony Blair introduced PFI . PFI remains a huge weight on many hospitals’ budgets. Blair and his government started propaganda for involving the private for-profit sector in the health service. Far from being more efficient, the for-profit sector has been damaging.
Carillion is just one example. The scandal of Carillion and the building of the Liverpool Royal Hospital will never be forgotten Privatisation has grown, especially under Coalition and Conservative governments who oppose the whole idea of the NHS and are privatising and breaking it to further open the way for big companies to profit at our expense.

What does NHS privatisation mean so far? ( Each of these initiatives means greater pain for patients.)
Before the pandemic, in 2019 privatisation was already eating into NHS resources, leaving it open to the catastrophe that followed
PFI – PrivateFinance Initiative – meaning that building new hospitals made a fortune for finance companies and huge debts for hospitals.
Outsourcing workers on lower pay and worse conditions
Contracts have been given to private companies to deliver some treatments, often at a lower quality than the NHS.
Hundreds of thousands of pounds are given to management consultants.
Services contracted out.
Government legal responsibility for healthcare has been removed.
There has been restructuring of the NHS into ICS so more of our tax money for health goes to private companies.
Patient data is included in trade deals.
Patients are being sent to private hospitals.
Migrants are being charged 150% of the cost of their NHS treatment meaning many people go without treatment or live in terrible debt.This policy has caused maternal deaths

The deaths of three pregnant women were directly linked to the Conservative government’s charging system in a major report that came out in December. The women died after delays in seeking help due to wrongly thinking they would have to pay for care.
Big Companies like Centene are taking over GP practices often reducing the level of care available.
Privatisation and cuts led to restricting treatments and creating waiting lists.
Hospitals, GP surgeries and maternity units were closed.
Mental health care is a tattered shadow of its former self.
Social care for people with disabilities and for our elders is privatised and charges service users.
Few NHS dental practices still function.
GPs are overworked and understaffed. Patients and staff are having to fight for their care.
“The UK spent around a fifth (18%) less on average than the EU14 on day-to-day health care costs” (the Health Foundation). The Government has decided not to adequately fund our NHS services. Seven million people are waiting for care and thousand are dying of preventable or treatable illnesses.
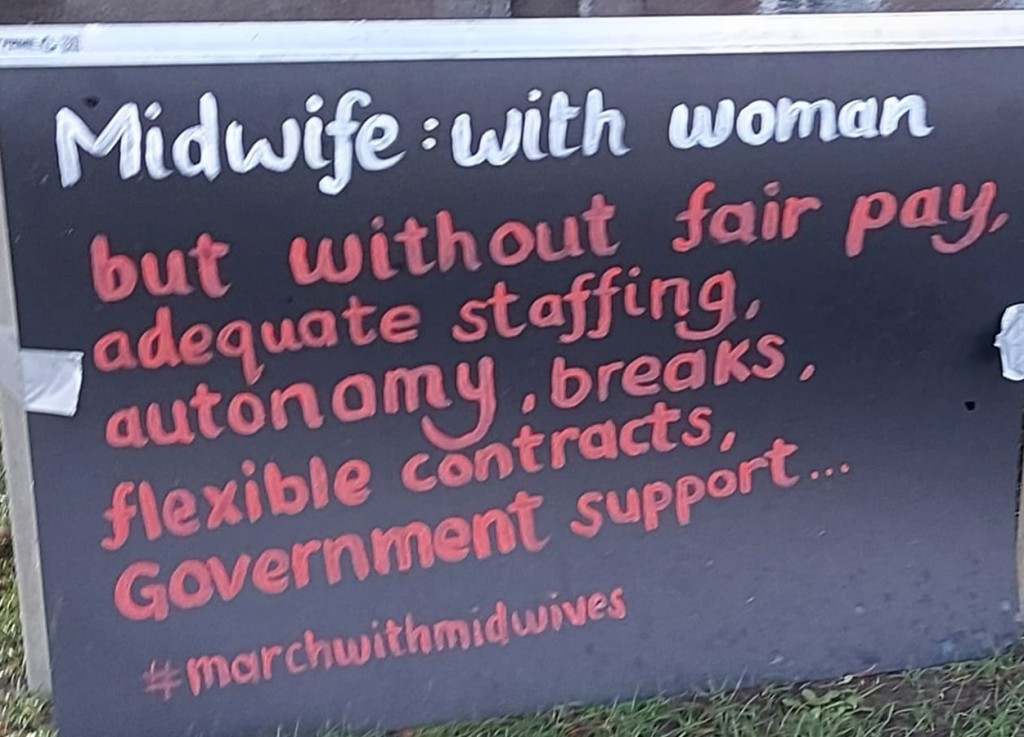
Staff in the NHS have seen their real terms pay decline for more than ten years, yet are overworked. The NHS is understaffed. We have fewer hospital beds than in similar countries and fewer doctors per head of population.

A system with fewer resources
The Kings Fund, a thinktank that has supported some recent “reforms”( and is certainly not left-wing) reported recently;

The UK has below-average health spending per person compared to peer countries. Health spending as a share of GDP (gross domestic product) was just below average in 2019 but rose to just above average in 2020 (the first year of the Covid-19 pandemic, which of course had a significant impact on the UK’s economic performance and spending on health services). The UK lags behind other countries in its capital investment, and has substantially fewer key physical resources than many of its peers, including CT and MRI scanners and hospital beds. The UK has strikingly low levels of key clinical staff, including doctors and nurses, and is heavily reliant on foreign-trained staff. Remuneration for some clinical staff groups also appears to be less competitive in the UK than in peer countries.
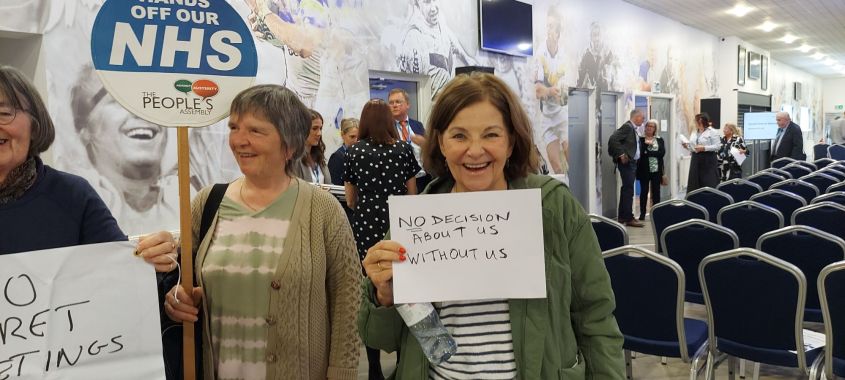
The NHS is broken up into 40+ ICS boards. Our ICS area is Cheshire and Merseyside. That is why the coordinated campaigns against NHS cuts and privatisation operates across Cheshire and Merseyside. We are all the local trade union councils, Defend our NHS, Keep our NHS Public, Save Liverpool Women’s Hospital, Merseyside Socialist Health Association and more.
You can join any of these groups or just the local group close to you. Email us at TakebacktheNHS@proton.me
Even now the government is imposing further cuts on the NHS. This is madness.
We invite you to join the Resistance:
to NHS privatisation
to poor pay, to denial of care, to underfunding, to endless waiting lists, to being forced to pay twice, to hospital and GP closures


Every tax pound that goes directly to health care repays itself many times over in the health of the economy as well as through the health and happiness of the people. Underfunding healthcare causes harm to the economy.

The campaign to save Liverpool Women’s Hospital and for better funding and better staffing of maternity services nationally and locally is crucial in Cheshire and Merseyside.
Liverpool Women’s Hospital serves women across Merseyside and Cheshire and beyond. 8,000 babies a year are born there. The hospital is the regional maternal medicine centre
Save Liverpool Women’s Hospital March
October 7th,2023, 12.30
Join the March for the NHS!
From Liverpool Women’s Hospital to Labour Party Conference at Liverpool’s waterfront.
Save Liverpool Women’s Hospital!
Save all the Hospitals under threat!
Restore and Repair the NHS!
Back to Bevan!
Support NHS staff!
Improve women’s healthcare.
Improve maternity care nationally


Talk to people about the NHS. Answer the Government’s lies. Spread the resistance. Demand restoration of the NHS.