We are not stopping until we win back the full NHS!
Wishing everyone a good Christmas and a great campaign in the new year
Save Liverpool Women’s Hospital.
Restore and Repair the whole NHS!
For all our mothers, sisters, daughters, friends and lovers and every precious baby.
- The UK still lags behind other wealthy countries in infant mortality.
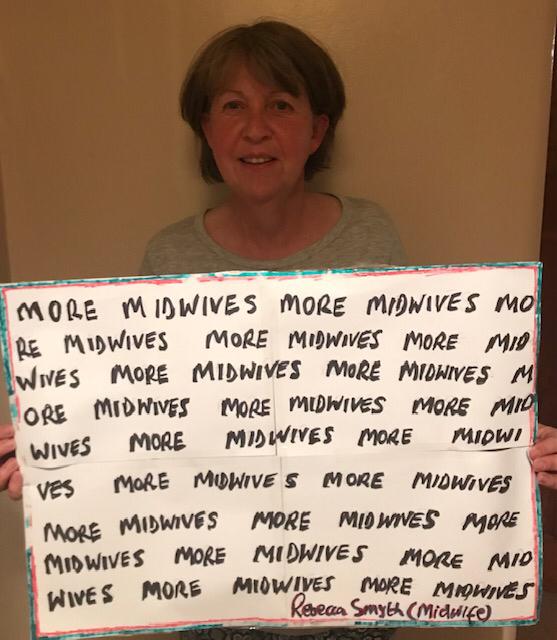
- Maternity is still grievously underfunded.
- Maternity is in crisis
- The health service is told to make further CIPs.
- Privatisation is burning through the NHS. Midwives and Nurses and Clinical Support workers are still underpaid and overworked.
There is no significant improvement in funding for the desperate NHS from the Government this autumn as they prepare for tax cuts for the very rich “ICSs told to prepare ‘nuclear’ service cuts as NHSE plays ‘hardball’.
The government cannot play ignorance. Their Chancellor Jeremy Hunt has been deep in the reorganisation of the NHS on US lines for years.
The government is provoking a huge crisis as we head into a winter of avoidable deaths and harm. It will make a pretty penny for the big corporations though.
We were promised consultation on the future of Liverpool Women’s Hospital but where is it?
Conveniently this appointment gets around the promised public consultation and to add to the murky mix the Liverpool Women’s Hospital will shortly share a Chair of the Board with Liverpool University Hospitals Trust ( The Royal Aintree and Broadgreen)
This is widely expected to be followed by a merger pulling women’s health, genetics, fertility, and maternity into a huge conglomerate.
Chief Executive of the Liverpool Women’s Hospital is the top Maternity job in the country. Maternity is in a national crisis of staffing and safety. Why won’t Mr Sumner tell us what he knows about Maternity?
Repeatedly, we see reports of inadequate care in maternity across the country. Most recently
“Maternity services at Royal Derby Hospital and Queens Hospital, part of University Hospitals of Derby and Burton, were inspected by the CQC in August as part of the regulator’s national maternity services inspection programme, which has seen an increasing number of maternity services across the English NHS rated “inadequate.”
Liverpool Women’s Hospital has also had a poor CQC report on maternity.
Liverpool Women’s Hospital claims to be the only fully staffed maternity provider in the country, though many of the midwives are newly qualified. We do hope those midwives stay!
It seems that the axe will not fall on maternity as hard as it will on other services.
Dr Suzanne Tyler, Executive Director of Trade Union at the RCM, said:
“While we acknowledge that this will be an incredibly difficult time for our colleagues elsewhere in the NHS, we are grateful that NHS England has listened to our plea to maintain the level of funding and investment in maternity services to protect safety. To have done otherwise would have been incredibly damaging to the ability of midwives, maternity support workers and other maternity staff to deliver safe care to women and families. We already know the impact that can have, and we are pleased to be working with Trusts and others to bring about positive change. This commitment to the continuation of funding should not be underestimated and we strongly urge Trusts to honour this commitment.
“Recent reviews by Dr Bill Kirkup and Donna Ockenden have called on the Government and on NHS bodies to address the chronic maternity workforce shortage and to invest in the safety of services. We hope that today’s announcement will go some way to make those recommendations a reality.”
Our campaign says “maintaining” current levels is not good enough and damaging the rest of the NHS is simply wrong Women need heart care, diabetes care, mental health care as well as maternity care and they all intertwine. Stop this government’s health policies in their entirety.
Women are being damaged.
Women, and especially mothers, are being damaged by poverty, the housing crisis cold homes and poor pay. Becoming a mother is very tough for many. A recent report shows young mothers are especially vulnerable.
Join your voices for our health care. Demand it back.
Restore and Repair the NHS. Stop the rot now!
Profit-centred policies are reshaping and downscaling our health services. These policies are destroying our services. providing fewer services, fewer beds and massive staff shortages. But it provides more profit for health corporations like Optum and management consultants like Carnall Farrar
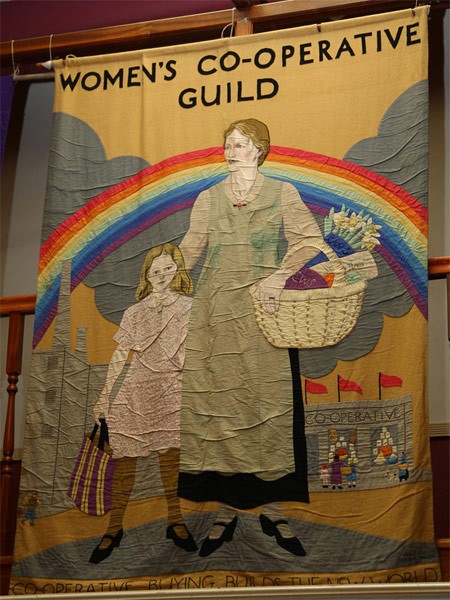
Privatisation policies are hidden behind sweet words. The privatisation lobby is also infecting Labour, so the fightback is down to us all. The NHS was not a gift from the great and the good but something fought for for years by working class women and by the Trade Nnions. We got the NHS that way and we can get it back the same way
Government policy costs lives., especially the lives of working-class people.
The US system has more preventable deaths than any other advanced country.

Fewer services are being provided in the NHS. Pressure is put on patients to use private healthcare. https://www.theguardian.com/society/2023/nov/26/one-in-seven-adults-in-england-advised-by-nhs-to-go-private
What has happened to dentistry and mental health services can happen to every service.
Wages and conditions in the NHS have fallen in real terms. Staff are working way beyond their duties just to keep the service afloat.
We will never get our services back unless we all spread the word.
Don’t be the person who has today to your grandchildren as they struggle to pay for poor health care
“Well we did have a health service for everyone but they privatised it”



Key facts
•In the US health insurance costs about as much as the family mortgage and does not cover everything. Many go without.
• Private healthcare cannot be as good as a national comprehensive service.
• We pay through our taxes. Government money invested in healthcare pays back into the economy.
Demand a return to the original NHS, once the best in the world. It was Government funded, providing timely healthcare for all, including all the services, publicly delivered by qualified staff with decent pay and conditions. This is how the NHS was designed by Aneurin Bevan, seventy five years ago.

It is the cheapest, most cost-efficient and humane way to provide health care. If YOU spread the word, we stand a chance of getting our services back .
We know we have the support of the people of Cheshire and Merseyside. We work with health campaign groups and trade unions across Cheshire and Merseyside and beyond. We have more than 70,000 signatures on our petition, combining the paper signatures and the online petition. We have distributed tens of thousands of leaflets; three big demonstrations all show this support.
We have a feral government intent on transforming the NHS into a cash cow for big corporations.
We are calling for a winter of protest and campaigns to inform the public. Help us if you can!

Contact savelwh@outlook.com
or