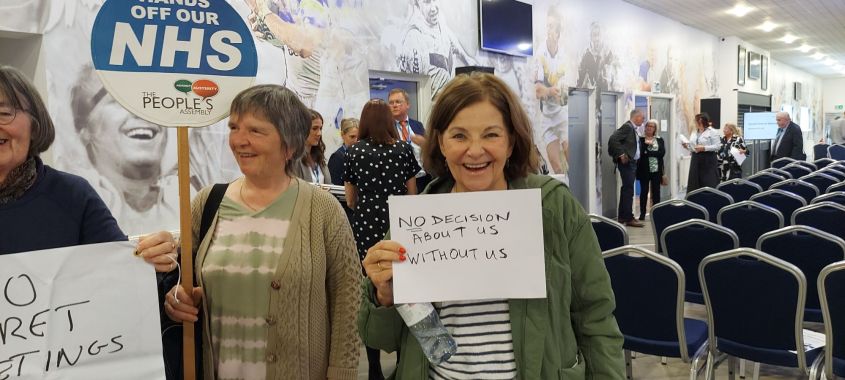
When Save Liverpool Women’s Hospital campaign are out and about people often ask about GPs. Why can’t they get appointments? Why don’t we know our GPs like we used to do? Why are some practices closed? Which bits are privatised? Why are some doctors unable to get work? Why are so many people who are not doctors employed at GP practices? Why, when need is increasing, are there fewer GP practices in England than at any time since 2016? Why are GPs in dispute with NHS England? Why are GPs so overworked? Why when people are less healthy do we have less healthcare?Why is less spent on GP practice than in 2018? If we want to Restore and Repair the NHS we need to know what has already happened to this much loved and very valuable service, what is happening now, what the privatisers have in store for us next and knowing all this we need to talk about how we can win it back.
Sheila Altes answers some of these questions. We welcome contributions to this discussion. The condition of the NHS means that many more patients and their families and friends need to know more.
General Practices
General Practitioner (GP) practices are not private companies, they are independent contractor organisations set up to deliver NHS services for the NHS. Staff working in general practice are usually employed directly by the GP practice and not by the NHS.
Every partnership of GPs must hold an NHS GP contract to run an NHS commissioned general practice. These set out mandatory requirements and services for all general practices as well as making provisions for several types of other services that practices may also provide if they choose to.(The Kings Fund 2020).
There are 3 types of contracts in England:
General Medical Services (GMS), Personal Medical Services (PMS) and Alternative Provider Medical Services (APMS).
The majority of GP practices hold GMS or PMS contracts.
General Medical Services (GMS)
GMS contracts are negotiated nationally every year between NHS England and the British Medical Association’s (BMA) General Practitioners Committee (GPC England). The GMS contract is then used by the commissioner to contract GP services in a geographical area to deliver ‘core’ medical services.
Personal Medical Services ( PMS)
This is another form of contract. Similar to the GMS but negotiated and agreed locally by the commissioner with a practice. It is soon to be phased out.
The core general practice contract sets out the geographical area the practice will cover. They must have a register of patients and provide the essential medical services set out in the contract. There are other requirements such as standards of premises and workforce and key roles and responsibilities including complaint procedures, insurance, liability and governance. They must provide essential services for registered patients and temporary residents who are or believe themselves to be:
*ill with a condition from which a recovery is expected
*terminally ill
*suffering from chronic disease.
They must provide ongoing treatment and care.
Alternative Provider Medical Services (APMS)
This new type of contract for the provision of NHS services was introduced in 2004. This allowed the contract to be held by a private company or a not- for- profit organisation; the contract no longer had to be between a named GP or GP partners and the NHS.
This effectively opened up primary care to private companies owned by directors and shareholders. So instead of GPs who had worked in an area for years, who knew their patients, primary care could be delivered by a private company who employed salaried GPs.
APMS contracts were advertised with a fixed amount of payment over a long term usually 10 years. As long as mandatory services were met and any services covered in the contract, then any money not spent was profit for the company and its shareholders. If the company or organisation held several contracts then economies of scale come into play (Lowdown 20/3/21). Further profits were made by down- skilling and reducing the workforce. These efficiency savings (cuts) don’t go to the NHS but to the shareholders.
This gave rise to the entrepreneurial GPs who set themselves up as directors of these companies and made huge sums of money. SSP Health comes to mind. In 2013 they took over the management of 22 surgeries in Liverpool. One of these surgeries was Princes Park Health Centre. Under their management it went from being a flagship model of primary care to being ranked in the bottom 300 out of 8000 GP surgeries in the country. A campaign by Keep Our NHS Public Merseyside focused on the difficulties of the patients at Princes Park. This campaign forced SSP Health out of Liverpool and their contracts for all but 2 of the surgeries were awarded to other providers. However they are still active in the North West and manage over 40 surgeries. Details of the KONP campaign can be found on:
www.labournet.net/other/1502/konp1.html
Even though the majority of GPs are independent contractors, the use of APMS contracts attracted many private companies who began to take over primary care.
Funding
GPs who hold a GMS or PMS contract are paid for services provided, both mandatory and additional services, where they have been agreed. Additional income is generated by the Quality Outcomes Framework (QOF). This is an incentive scheme that allows practices to earn points for performance of good practice, Achievement is measured for indicators in 4 areas known as ‘domains’: Clinical Domain, Organisational Domain, Patient Experience Domain and Additional Services Domain.
In the clinical domain, there are approximately 20 areas where points can be achieved. For example, registers of patients with long term conditions such as : asthma, chronic obstructive pulmonary disease, chronic renal disease, cardiovascular disease, hypertension, diabetes etc. If a certain percentage of these patients are reviewed annually and are found to be on the appropriate medication for their condition or if control of their condition is achieved within guidelines set out by NICE, then points are awarded and payments made.
The system is open to abuse and can become a box- ticking exercise. Unscrupulous practices can manipulate the registers remotely.
This system is operational in England, Northern Ireland and Wales. Changes to the framework for 2023/24 were imposed by NHS England but rejected by GPC England and NHS England has committed to a review of the system. More information can be found at:
Quality and outcomes framework (QOF) www.bma.org.uk
Money is also paid based on the size of the practice population and “weighted” according to certain criteria. The average payment per” weighted patient” was £104.73 in 2023 (NHS England).
“Weighted” list size is a measure of workload on the basis that it represents a measure of time expected to be spent on consulting. Certain types of patients place a higher demand on practices than others, for example: elderly patients, patients with mental health issues, non-English speaking patients, or if the practice is in a deprived area where patients are more likely to have complex conditions.
The practice must pay all its salaried employees and the running costs of the practice. The partners do not get a salary but get paid out of the practice income. They are also liable for any losses made by the practice.
Further funding was made available to general practices if they became part of a Primary Care Network.
Primary Care Networks (PCN)
PCNs were introduced in England as part of the NHS Long Term Plan published in February 2019.
A PCN consists of several general practices working together, so instead of a general practice caring for a few thousand patients a PCN will have between 30,000 and 50,000 patients on its list. Each PCN will have its own Clinical Director, who doesn’t have to be a GP. Governance structures will be determined locally and recorded as part of a Network Agreement. Funding will be made available to GP practices in PCNs via the Network Contract Directed Enhanced Service (DES).The contract will be in addition to existing GMS,PMS and APMS The contract will be between the commissioners and the individual practices and the money will be channelled through a single bank account directed by the network.
Additional staffing will be required to deliver the seven National Service specifications of the DES. They are:
*structured medication reviews
*enhanced health in care homes
*anticipatory care (support that focuses on people with long term conditions with the aim of reducing the risk of their condition worsening that would result in a hospital admission)
*personalised care ( patients have more choice in the way their care is planned)
*supporting early cancer diagnosis
*cardiovascular disease case finding
*action to tackle inequalities.
The additional staff needed included physician associates, first contact physiotherapists, social prescribing link workers and clinical pharmacists. Funding is given for these via the Additional Roles Reimbursement Scheme (ARRS). Underfunded and understaffed general practices cannot use these funds to employ other GPs, with the result that many salaried GPs and locums cannot find employment.
Digital -first primary care became a new option for every patient, they would have the right to choose telephone or on- line consultations instead of face- to- face consultations. This could be with their own practice or a digital provider. A framework was created for digital suppliers to offer their services to networks on standard NHS terms. This represented a golden opportunity for software companies to jump on the bandwagon and also to access patient data, invaluable to health insurance companies.

The Long Term Plan was published in February 2019 and PCNs were to be formed by June 2019. Forcing successful and struggling practices into networks in such a short time did not give them the support needed to deliver priorities: all part of the plan. NHS England then published a list of approved suppliers of support and development available on the Health Services Support Framework. They included: Centene, Virgin Care, Optum, KPMG, Deloitte, Ernst & Young, PwC, McKinsey, Cerner, Atos and many more global corporations. This proves the intention is to stream NHS public funds into these corporations (Green,J.,2019)
The aim was to cut GP appointments and also the number of GPs needed to care for patients. Only patients with complex needs will see a GP, the rest will be sign posted by a “care navigator” to less skilled clinical staff.
Investment and Impact Funding (IIF) is another source of funding linked to networks rather than practices. The fund is an incentive scheme focusing on supporting PCNs to deliver high quality care; there are indicators that focus on where PCNs can achieve this. In 2023, the number of indicators was reduced from 32 to 5. Payments were made if the PCN achieved a certain percentage of people receiving flu jabs, learning disability health checks, fast track referrals for lower gastrointestinal cancer and patients being seen within 2 weeks of booking an appointment. This reduction in indicators freed up funds to be moved to the Capacity and Access Payments. to facilitate the Same Day Access scheme.
In this scheme, when a patient phones the GP practice, they will be put through to a centrally controlled system. If they want a same day appointment the call will be transferred to a Same Day hub where a ‘care coordinator’, not a doctor, will triage the patient on to someone else at the hub, also not a doctor, who will decide how to deal with the request. Each hub will be staffed by physician associates and only one senior supervising GP.
This caused serious concerns in North West London, where the scheme was being forced on the PCN from 1st April 2024. They were concerned that the plan could potentially cause serious threats to patient safety and could lead to the replacement of fully trained GPs by cheaper, less well trained staff (GP Direct. February, 2024). Patients could be sent anywhere within the group of networks, which would make continuity of care difficult. There is increasing evidence that a high level of continuity of care results in better health outcomes (NICE. February 2019)
The plan had been designed by KPMG, one of the 4 big accountancy multinationals, paid to design it and to train GPs how to use the service. No patients, residents and a minority of GPs were consulted. After a huge backlash the North West London ICB were forced to retreat but did not abandon the plan, only to introduce it more cautiously (Health Campaigns Together, Spring 2024).
PCN Incorporation.
PCNs are not legal entities. They cannot hold contracts, employ staff or own property. This means there is no corporate model, it is the practices themselves that have to enter these arrangements on behalf of the network. Rather than have a lead practice employing staff and managing funds on behalf of the other practices, a corporate vehicle can be used to manage PCN activity and funding between members.
Forming a corporate vehicle involves merging the PCN practices into a single practice. In this way they can become limited companies with shareholders. Once the corporation vehicle is formed, assets, staff and contracts can be transferred into the corporate vehicle.
The corporate vehicle may provide administrative activities or could sub-contract responsibility for clinical services delivered under the DES contract. It can enter contracts in its own right, own property and be responsible for employing staff.
If networks are forced to merge, as outlined in the North West London plan for Same Day Access hubs, then a company can be formed via a corporate vehicle. This is an attractive opportunity for private equity firms to invest in the company as income from the NHS is virtually guaranteed. In order to make a profit, private equity companies invest in companies for a limited period, they then restructure it and make efficiency savings, usually by reducing services, cutting corners and reducing staff. They fund the investment partly with their own investors’ money and by borrowing. Once the contract ends, they share the profits with their investors and pay off the debt. Depending on the contract they often leave the debt with the company invested in. Private equity companies don’t have shareholders so there is little transparency.
The responsibilities of GPs in the UK have increased, partly due to the austerity imposed by the Government in the last 10 years. Income inequality affects health, and poor health puts a greater demand on healthcare. The reduction of bed capacity in secondary care, causing ever increasing waiting lists adds more pressure on GPs as they care for patients awaiting hospital treatments (Pulse 4/10/2023).
The extra administrative work necessary to obtain funding adds to the pressure on GPs .The new GP contract proposal for 2024/25 will see an uplift of only 1.9%, while, according to local intelligence, overheads have increased by 15%.
Dr. Katie Bramall-Stainer, chair of GPC England, states in response to the new GP contract proposal:
“They know as well as we do, that can only mean practice closures, staff redundancies, loss of the GP workforce, fewer GP Nurses, reduced activity, reduced access and an unacceptable experience for patients” ( BMA 28/2/2024)
By understaffing, underfunding and overstretching primary care, it is little wonder that the numbers of GPs has fallen. There needs to be a recruitment and retention of GPs, adequate funding and an end to private providers in the NHS. We need to continue with our campaigning to restore our NHS to its original founding principles of a universal health service, funded by taxation and based on need and not the ability to pay.
Sheila Altes April 2024.
REFERENCES
British Medical Association (BMA) 28th February 2024
Responding to the new GP contract for 2024/25
British Medical Association
Quality and Outcomes Framework (QOF)
Changes to the framework in England 2023/24
GP Direct
Same Day Access Hub Proposal- February 2024
Green, J. 2019
Large scale integrated primary care networks.
http//:calderdaleandkirklees999callforthenhs.wordpress.co
Health Campaigns Together – Spring 2024
Row over exclusion of GPs from ‘improved’ GP services in NW London.
GPs across the world- why do GPs have the most stress despite not working the most time.
Pulse 4th October 2023
NHS England
Health Systems Support Framework
NHS England
Managing regulatory and contract variations.
National Institute for Health (NIH)
Calculating adjusted weight list sizes
The King’s Fund – 11th June 2020
GP funding and contracts explained.
The Lowdown -6th October 2023
Private equity investing in UK healthcare
The National Institute for Health and Care (NICE) 2019
Continuity of Care and Support.