Good health care makes a country richer, healthier and happier. It is an excellent investment. Good healthcare gives exceptionally good returns for each pound spent, both financially and socially. Good healthcare gives babies a great start in life, saves the lives of babies and the health of their mothers, and prevents long-term damage to health.
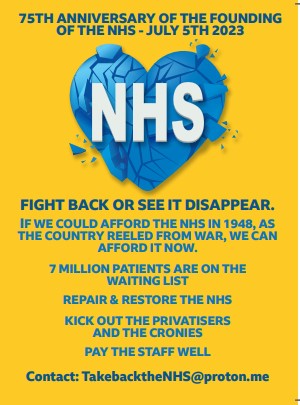
Universal healthcare free at the point of need, run as a not-for-profit, national system, and publicly delivered is by far the most economical and cost-effective way of delivering healthcare. This is the original NHS model.
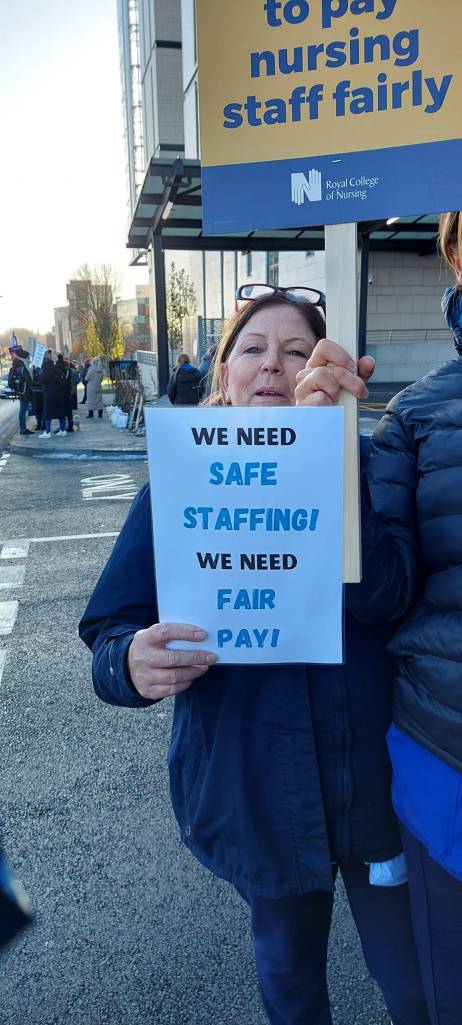
Good pay for healthcare workers helps the health system work well, helps the economy grow, protects the physical and mental health of the workers, reduces the need for means-tested welfare and reduces poverty. It also says to those workers, your work is valuable, essential and complex requiring great skill and an abundance of care. Good pay should be a way of saying thank you to medical and healthcare workers.
Good healthcare grows the economy, helps sustainability. It is not a drain on the economy.
Market-based healthcare, as seen in the USA and as being sneaked into our NHS, makes corporations wealthier and happier and damages our health, our society, our communities and the economy.
“NHS will be just a memory!” one young woman said as she signed our petition.
Why is the health service starved of funds? Why is money haemorrhaging out of it into private companies?
There are intertwined issues making up the background to the threats to Liverpool Women’s Hospital. This list does not imply an order of priority; each issue is important in itself:
1. The chronic neglect of women’s health issues for many years, as well described in many reports, culminating in the Government’s Women’s Health Strategy which says:
The Women’s Health Strategy promises to address the poor experiences and worse health outcomes that women endure. The underlying cause of these issues is that the health system has historically been built by men for men. Consequently, women are often not listened to or believed by the health and care system. So, the crucial question is, will this strategy change the culture in the NHS of women not being listened to about their health and wellbeing?
2. The acute underfunding of healthcare which leaves hospitals struggling and their management focussed on balancing the books.
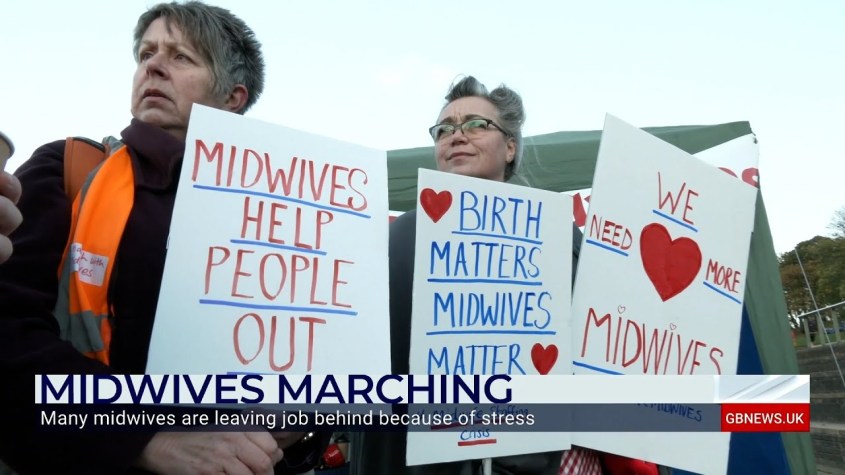
3. The Maternity Crisis. The experience of giving birth is deteriorating as cuts bite. Our Midwives and other maternity staff strain every sinew to provide good maternity care but there are too few midwives, too few obstetricians and gynaecologists. They are overworked and underpaid. The country is short of midwives “Midwives are being driven out of the NHS by understaffing and fears they can’t deliver safe care to women in the current system, according to a new survey of its members by the Royal College of Midwives (RCM)”. Maternity is underfunded. The maternity tariff (the money the government allocates to maternity) is inadequate.
Infant mortality is worse in the UK than in 37 other advanced countries There has been a series of reports on the tragedies coming from the problems in maternity. We are worse than 39 other countries in maternal deaths.
Even this week there were further reports of problems in maternity care “Leaders of two maternity services have been told to take urgent action, after inspectors found understaffing and declining levels of care, despite safety warnings from midwives.
Maternity services at University Hospital North Durham and Darlington Memorial Hospital have been downgraded from “good” to “inadequate” in Care Quality Commission reports, published today. The CQC noted a “concerning deterioration” in the care the two services provided, despite midwives telling managers they felt the service was unsafe.”
There are severe problems with mental health services linked to maternity.
We can see the terrible maternity scandals. Our love and sympathies to all the babies, mothers, fathers and families involved and all the staff who did their best to challenge the situation. We honour you in our fight for a better health service and better care for maternity and women’s health.
4. The pattern of concentrating resources in big hospitals which, until the Ockendon Report did not even have to have a Maternity Champion on their Trust board. A big hospital does not cause the deaths, nor does that model prevent these tragedies. Respecting women, respecting the working classpeople, respecting ethnic minorities, respecting patients and the public all would help prevent these deaths, and we see precious little of that in the situation in Liverpool, Cheshire and Merseyside.
5. Money. Maternity care is nationally underfunded but no other hospital has such a large part of its income dependent on the maternity tariff so this affects particularly Liverpool Women’s Hospital.
6 Staffing problems, caused by poor pay, underfunding, using vacancies as a way of saving money and by staff leaving maternity nationally because of unmanageable work pressures and poor pay.
7. The cost of the Foundation Trust administration requirements.
8. Underfunding which denies the Liverpool Women’s Hospital the full range of intensive care services, requiring about eight women a year to be transferred one mile away to Liverpool Royal for intensive care. Many women are transferred into Liverpool Women’s Hospital as well. Transfers between hospitals are routine but complicated by the internal market in the NHS and of course years of underfunding.
9. The difficulties in cooperation between hospitals as imposed on the NHS by the 2012 Health and Care Act where hospitals were supposed to act like competing companies in a market, rather than components of an integrated and cooperative national service.
10. The huge waiting lists for treatment.
The British Medical Association (BMA) says “…around 7.68 million people waiting for treatment, an increase from the previous month; nearly 3.18 million of these patients waiting over 18 weeks; around 390,000 of these patients waiting over a year for treatment – which is around 308 times as many as in July 2019, before the pandemic began”. This is the equivalent of the whole population of the North West of England. There is also a hidden waiting list caused by non-referrals or difficulties in getting to see a GP.
11. Waiting in A & E is a big problem as seen in this Blackpool death.
“Harold Pedley, known as Derek, attended his GP surgery during the late afternoon on 21.12.22 and after spending most of that day feeling unwell with symptoms including abdominal pain and vomiting. He was appropriately referred to the hospital and travelled there with his Friend after his GP had discussed his case with doctors. Due to a lack of available beds in the assessment unit, Derek needed to remain in the emergency department. Following his arrival at 20.07 hours, doctors were not notified of his attendance. He remained in the emergency department waiting area for almost two hours during which time due to significant pressures faced by the department he was not assessed or spoken to by a medical professional. At 21.59 hours a triage nurse called for him. By then, Derek had been unresponsive for some time and had died, his death confirmed at 22.26 hours. A subsequent post mortem examination revealed he died from the effects of non-survivable extensive small bowel ischaemia caused by a significantly narrowed mesenteric artery. His death was contributed to by heart disease.
“At the time Derek arrived, as the Hospital Trust’s own internal review of this death explained, such were the pressures on the hospital Trust posed by patient numbers that it was operating at OPEL [Operations Pressure Escalation Level] 4. This is a method used by the NHS to measure the stress, demands, and pressure a hospital is under. OPEL 4 represents the highest level, when a hospital is “unable to deliver comprehensive care, and patient safety is at risk”. This is not a ‘one off’ event, and such pressures are becoming ever more common.
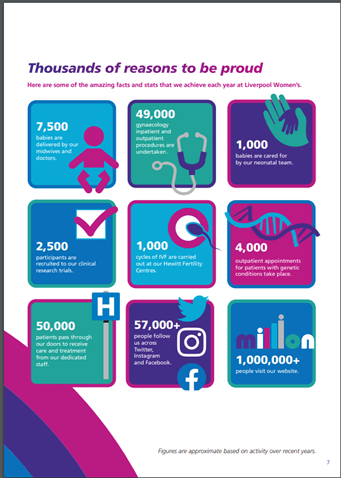
Liverpool Women’s Hospital reports that;
The urgent and emergency care (UEC) system continues to experience significant pressure across the whole of NHS Cheshire & Merseyside, with the majority of trusts across C&M consistently reporting at OPEL 3 in 2023 to date. The system has been escalated overall at OPEL 3, which is defined as ‘the local health and social care system is experiencing major pressures compromising patient flow‘. And this is in Summer.
12. Women are again faring badly on waiting lists. Health Watch reports that
- Women are 28% more likely to wait over four months for NHS treatment than men (54% vs 42%).
- More women are also likely to experience adverse impacts of long waits compared to men.
- Most strikingly, women are 50% more likely to say that long waits impacted their ability to socialise than men (41% vs 28%).
- Thirty-eight percent of respondents who identified as female said that waiting for treatment impacted on their ability to work, compared to male respondents (29%).
“More than half a million women face prolonged waits for gynaecology care.”

“Women face extreme pain, heavy bleeding, and poor mental health as waiting lists reach record numbers” (From the Royal College of Obstetricians and Gynaecologists. April 2022).
Poorer people and people from ethnic minorities also suffered worse than average. Women, poorer people, ethnic minorities and disabled people are part of the demographic of Liverpool and Liverpool Women’s Hospital, so this should be a factor in decision making.
13. Treatments, like dentistry, opticians, hearing aids, where now we must pay individually or do without.
14. Misogyny in the NHS. Seventy-seven per cent of the NHS workforce is female, but still there is a gender pay gap and men overall are paid more than women and are more likely to be in senior roles. The women in the NHS are amongst the most educated and dedicated in the county and yet are still subjected to sexual assault, bullying and discrimination.
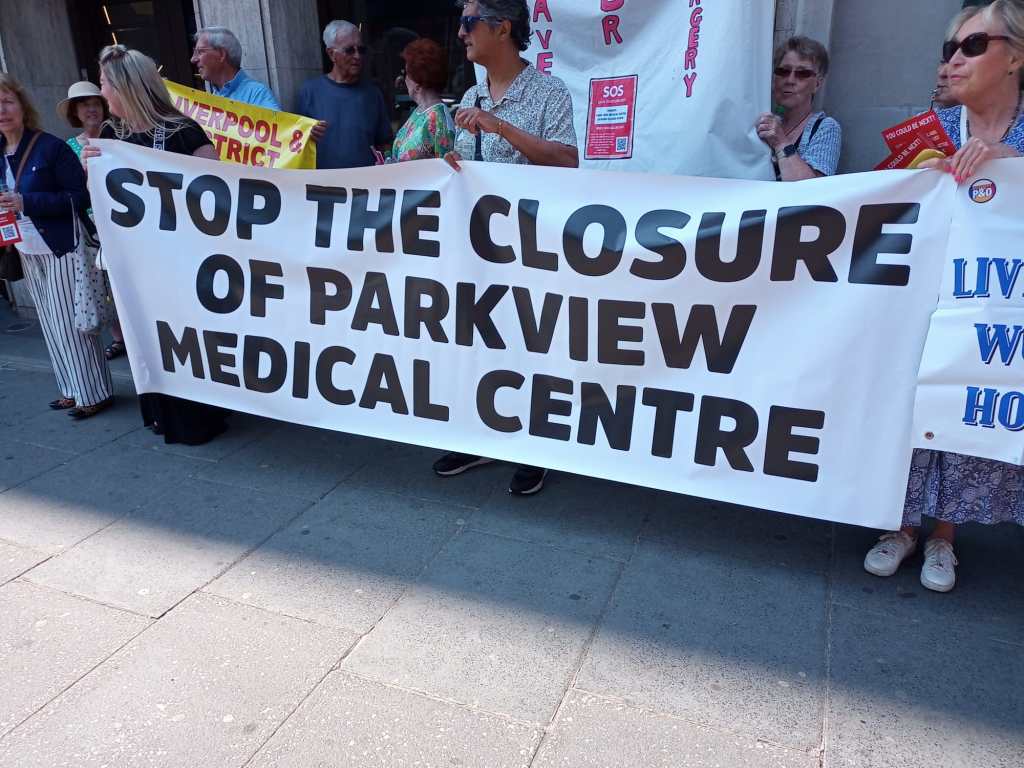
15. Disrespect towards Liverpool’s pattern of specialist hospitals, a pattern which is based on the history of the city and its role as one of the core cities of the region, and beyond. We have some wonderful specialist hospitals in Liverpool Including the Liverpool Women’s Hospital, the Heart and Chest Hospital, the Walton Centre for Neurology and Alder Hey Children’s Hospital. The Liverpool Echo reported on the threats to them here and we reported this in our posts about the Carnall Farrar report.
16. Mental Health. The privatisation of so much of our mental health services, coming alongside the pressures of years of Austerity, rising poverty, and the cost of living crisis, heaps ever more pressure onto working-class communities. We used to have good Child and adolescent mental health services, but now the service is a shadow of its former self and our children are suffering.
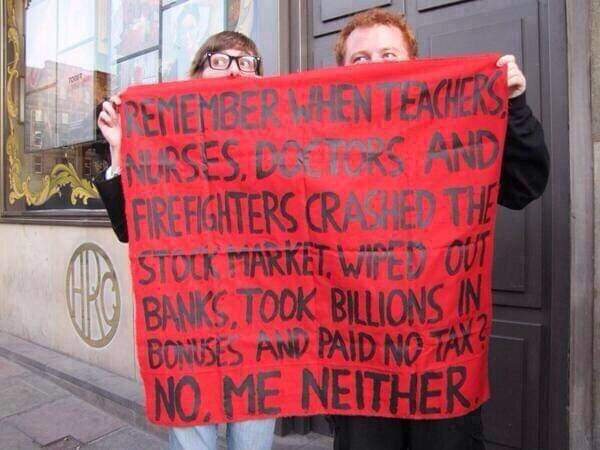
17. Staff shortages and staff pay. Staff have been on strike over pay and over working conditions and about restoring the NHS. We must heed their warnings about the state of the NHS. Consultants and Junior doctors are about to strike again. Industrial action has cost the government far more than if they had met the pay claims. This government is ideologically anti-union and anti-NHS.
18. And above all the long-term drive to privatisation, the introduction of the American model of Accountable Care which envisages less care in hospitals, denying certain services, for example, breast reduction, which the NHS declared to be of no clinical worth(!)and outsourcing many other services to private companies. This culminated in the imposition of the Integrated Care System. In our view the ICS is not integrated, is not taking Care, breaks the national system, hands vast sums of money to the private sector, and makes huge cuts in finances. We listed local examples here.)

19. The austerity politics of healthcare. Political parties that support Austerity pretend that the country cannot afford healthcare. We say, as do many economists, that money spent on healthcare (if that money gets to patient care and to staffing), makes the country richer because it keeps workers working and makes recovery quicker. It happens to help more babies live as well. Deaths caused by Austerity rarely get a mention in NHS papers but it is referred to in the House of Lords Library, where it says “approximately 335,000 additional deaths had occurred between 2012 and 2019 compared with what had been previously been predicted. It also said the change in these trends was greater for people living in the 20% most deprived areas in England, Scotland and Wales.” Of the deliberately limited spend on health care since Austerity started, far too much of our tax pound goes to private companies and private medicine.

20. The impact of the privatisation lobby has been enormous, penetrating the thinking of political parties and even some who work in healthcare. Our Lobby for the NHS, for treatment free at the point of need, publicly delivered, publicly owned has got to be larger and louder., has to get deep into the unions, workplaces and communities.

This blog is written from the standpoint of the campaigns in Cheshire and Merseyside but we love working with other campaigns for the NHS.
Please do sign our petition and please come on our demonstration