
We didn’t say it would be easy to do so but it’s definitely possible if people keep coming forward to help.
This is a report on the immediate situation. Another blog will look in detail at the background factors
The board of Liverpool Women’s Hospital and, we presume the ICB, have agreed on the appointment of a joint Chief Executive Officer with Liverpool University Hospitals NHS Foundation Trust. We believe this appointment is a first step towards a merger and the dispersal of services. It is normal for a merger to follow such an appointment.
The original job advertisement for the new CEO of Liverpool Women’s Hospital said this and included the graphics shown here.
“Liverpool Women’s NHS Foundation Trust delivers the highest standards of care for women, babies, and families. Each year we deliver over 7,500 babies, carry out over 49,000 gynaecological inpatient and outpatient procedures, care for over 1,000 poorly & preterm newborns, perform around 1,000 IVF cycles and have over 4,000 genetic appointments taking place. We believe that this along with a strong dedication to research & innovation makes us the specialist health provider of choice in Europe for women, babies and families.“
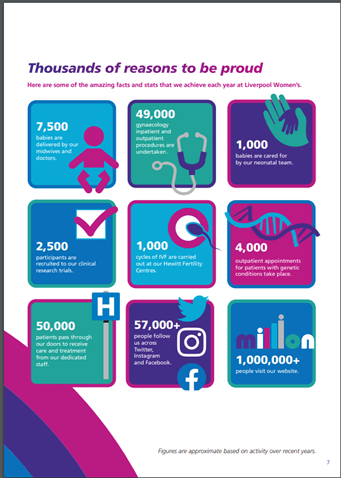
We have some of the leading experts in their field, which has been showcased on national TV and news, making our teams famous across the world for professionalism, skill & compassion.”
“…..the only specialist trust for women and babies in the UK and the largest standalone women’s hospital of its kind”
We want to keep this hospital, for all our mothers, daughters, sisters, friends, lovers, and every baby born there.
Among the person specifications for the CEO role was:
“Demonstrable and detailed understanding of current women’s health issues, national policy and standards, as well as best practice locally, nationally and internationally.”
We would love to know how the board considered that the CEO of Liverpool University Hospital Foundation Trust met these criteria. Maternity at his previous hospital Mid Cheshire Hospitals NHS Foundation Trust was evaluated by CQC as “requires improvement” though this may have happened before he got there. Over a number of years, there were eleven temporary closures of the Maternity Unit at Mid Cheshire. One woman in labour was turned away from the hospital due to a lack of beds. This is not reassuring. He might have dramatically improved maternity and women’s services there but we have not been able to find evidence of this.
Join us on the 7th of October in our demonstration. Act before the NHS is merely a memory.

More than seventy-three thousand people have signed our petition to Save Liverpool Women’s Hospital and to repair and restore the NHS. The petition is online here and on paper at our stalls. We get great support on the streets for our campaign. Our campaign, and similar campaigns across the country continue. We need to reach more and more people and organize people to speak up.
Even as the NHS is being stripped away, much great work is still being done, day after day, in our hospitals, clinics, and GP practices thanks to our healthcare workers. Our NHS workers have kept the ship afloat throughout the years of cuts.

Recent local developments in the battle for the NHS, for safety in maternity, and for women’s and babies’ health. On the 14th of October, the Liverpool Women’s Hospital Board met. Members of the public attending heard of some great work, and of many problems.
The board considered developments in the role of Maternal Medicine Centres, a new development. Liverpool Women’s Hospital is one of three Maternal Medicine Centres in the Northwest.
“The Maternal Medicine Centres will provide a regional service including pre-pregnancy, antenatal and postnatal care for women who have either pre-existing significant medical problems or medical problems arising in or shortly after pregnancy. The MMCs will also provide advice and care for the most complex and highest risk women including those with respiratory, haematological, renal and cardiac problems and women diagnosed with cancer. “
The board also heard a patient’s story which has helped develop innovations in menopause care, including having some joint menopause and mental health clinics. The attention now being paid to menopause is a great step forward and is disclosing years when treatments were simply not available leading to women’s long-term ill health. The patient’s story showed how women staff, nurses and doctors, can work together and push through real change. Surely this cooperation and mutual respect is much easier in a women’s hospital rather than in a huge four-site hospital. Will the new CEO prioritize the forty-odd people waiting in A and E for a bed at the Royal site, or agree to these innovative clinics?
Delays in Induction of labour. The meeting also discussed problems at the hospital with women kept waiting for Induction of Labour. This was both a staffing and a space issue. Induction of Labour is used for safety reasons so delays are potentially dangerous.”Delay in the induction of labour (IOL) process is associated with poor patient experience and adverse perinatal outcome.” Studies have shown this happens more in planned Induction of Labour rather than when the induction is an emergency
The board also received a brief report from the Letby case but could not discuss it in detail, because of ongoing police investigations.
As members of the public, some of our campaigners have attended board meetings for many years. We cannot contribute at these meetings but we can ask questions at the end of the meeting. On September 14th there was the first board meeting since the announcement of the intention to install a shared CEO between Liverpool University Hospital Foundation Trust and Liverpool Women’s Hospital. This issue of a shared CEO had not been raised in the previous Board papers. The author asked if campaigners had missed some paperwork about this and we were told no, we had not. At the previous meeting, the discussion was about putting an advertisement out for a new CEO.
Announcing a shared CEO is a fundamental change. We had been assured of public consultation on the future of the hospital but this critical decision happened without consultation and without being mentioned at previous board meetings. It happened after we were told in multiple meetings that decisions about the future of Liverpool Women’s Hospital were to be made via the Women’s Committee of the ICS.
Confusion has deepened.
It seems, from the board meeting, that the advertising and recruitment were managed by the Remuneration Committee at Liverpool Women’s Hospital, for which minutes are not published. According to the Chair of the Board, in a verbal answer, they had approached the ICB and system partners about the possibility of a joint CEO some time previously. (Again, we cannot find this in the public papers). They had been told that the time was not right so had gone on with the advertising for a new Chief Executive. Then they were told (It is not clear by whom) that the time for this joint CEO was now right, so they ceased the advertising process, closed the vacancy, and agreed to the joint appointment. Did the board, staff, and concerned patients at LUHFT know about this before it happened?
Who is making these decisions? Where is the clarity? Where is the candour? Where are the impact assessments? How can the public follow this?
We were told that the report from the chair of the Women’s Committee of the ICB had arrived too late for the Board papers but it has been on the ICB website since the beginning of the month. How moving to a shared CEO matches with this report from the chair of the ICB Women’s Committee beats me. The report says, “This committee will oversee the development of a safe and sustainable future model for women’s health services in Liverpool” Did it oversee the idea of a joint CEO? If so, why were we specifically told otherwise?
There are serious money troubles at both Liverpool Women’s Hospital and Liverpool University Hospital Foundation Trust. In the minutes of the previous meeting, there was this statement
“It was asserted that wider system support would be required to find solutions for the structural deficit that underpinned the Trust’s financial challenges”.
This “wider system support” means that more money from the local ICB and the system of hospitals it controls will be needed.
At the board, the severe financial pressures of the hospital were partly discussed in the “in public” section of the meeting and were due to be discussed in depth in the afternoon private session. The financial problems of Liverpool Women’s and Liverpool University Foundation Hospitals Trust are severe yet they are expected to make more than five per cent CIPs (cuts) plus making good non-recurrent savings made last year. There are money problems also in Mersey Care, and the Countess of Chester. This is not spendthrift hospitals but structural underfunding and a government bent on cuts.
Finances at the Women’s
The core issues specific to Liverpool Women’s Hospital are.
Nationally inadequate NHS Funding.
Inadequate funding for maternity through the maternity tariff. This affects all maternity providers but the scale of maternity at LWH makes it a far greater problem.
The cost of running a Foundation Trust
The Insurance system which is based on market models and which nationally carries more claims from maternity than any other service.
The inclusion of nonrecurrent items in balancing last year’s books. The government has insisted this is made good across the country.
Making between five and six per cent CIPs(cuts).
Cuts in spending inevitably impact staff pay and recruitment because that is where most of the budget is spent
Winter is coming.
Each doctor or nurse with whom I have informally discussed this situation, says that the situation this coming winter fills them with fear. We must demand better funding, money directed exclusively to staff and patients, not to privatization.
Our local hospitals are already under pressure in summer and early autumn. Most local hospitals even in the summer were reporting that they were on Opel 3. This is reported on page 23 of the board papers. What does this mean? The NHS says
At OPEL 1, there is a low level of pressure on NHS services, and the system is functioning normally.
- At OPEL 2, there is moderate pressure, and healthcare facilities may need to take additional steps to manage demand and capacity.
- At OPEL 3, there is a high level of pressure, and the system may need to implement additional measures such as canceling elective surgeries or diverting patients to other facilities.
- At OPEL 4, there is severe pressure, and the system is at risk of breaking down.
- At OPEL 5, there is a critical level of pressure, and the system is unable to deliver comprehensive care.
We need action for the health service now and not one penny must be diverted from patient care, staff costs, and building and estate safety before the winter sets in.
In summary, we want to keep Liverpool Women’s Hospital as a standalone Hospital, cooperating and working in a mutually respectful system across the whole NHS. We want to keep our specialist hospitals too. As our petition says “Save the Liverpool Women’s Hospital. No closure. No privatization. No cuts. No merger. Reorganise the funding structures, not the hospital. Our babies and mothers our sick women deserve the very best”.
Liverpool Women’s Hospital is much valued by the people of Liverpool. For many years now its future has been under threat. Nationally many hospitals are also under threat and many have closed. There is no evidence that closing swathes of hospitals improves healthcare. Our health has been declining in this time of closures. There is no evidence that huge reorganizations are more effective. Necessary reorganisations are damaged if implemented without resources. Everything we face at Liverpool Women’s is reflected in the rest of the country.
We must fight to save our healthcare. Fight for our rights, for our lives.
Every worthwhile right that we have ever won, had to be won, first, in the minds of the people. This includes the vote, equal pay, maternity leave, free and universal education, abortion rights, race equality, effective sewers, trade union rights, and some level of environmental protection. LGBT rights, ending slavery, all of them. The idea of healthcare, universal, free at the point of need, as a public service, funded by the government was first won in the minds of the public, by working-class women and trade unionists (and, back in those days, the Labour Party), before the post-war Labour government introduced it 75 years ago.
The people of Cheshire and Merseyside and beyond, the women and families in, the UK are entitled to world-class healthcare. Our communities have paid for the NHS for 75 years, and we continue to pay our taxes and our National Insurance, contributing far more as a percentage of our income than the rich do), but the government does not release the money or diverts it to the private sector.
We must protect what’s left of our healthcare, we support our healthcare workers, and demand the return of what has been taken from us to fill the coffers of big corporations.
The Government is implementing fundamental change to the NHS, change that no one voted for, change that was in no party’s manifesto, but change that makes the corporations and some of the ultra-rich even richer. This change is obscured by a smokescreen of propaganda coordinated by a lobby group that makes the tobacco and Oil lobbies look like amateurs. They seem to have their tentacles into parts of the Labour Party too. These changes are costing lives and pain for ordinary people.

We are entitled to know what is happening to our healthcare. Who is making what decision? Where are they making these decisions? What is the reasoning behind decisions being made? What impact assessments have been done? How and when is the public allowed a say? Where is the candour??

