This is a deliberately detailed post. A shorter version is available here

Major changes to the governance of all the hospitals in Liverpool (except Alder Hey Children’s Hospital) have been announced. This sounds quite boring but it is a symptom of a deeper problem, affecting our NHS, locally, regionally and nationally.
It directly affects the future of Liverpool Women’s Hospital.
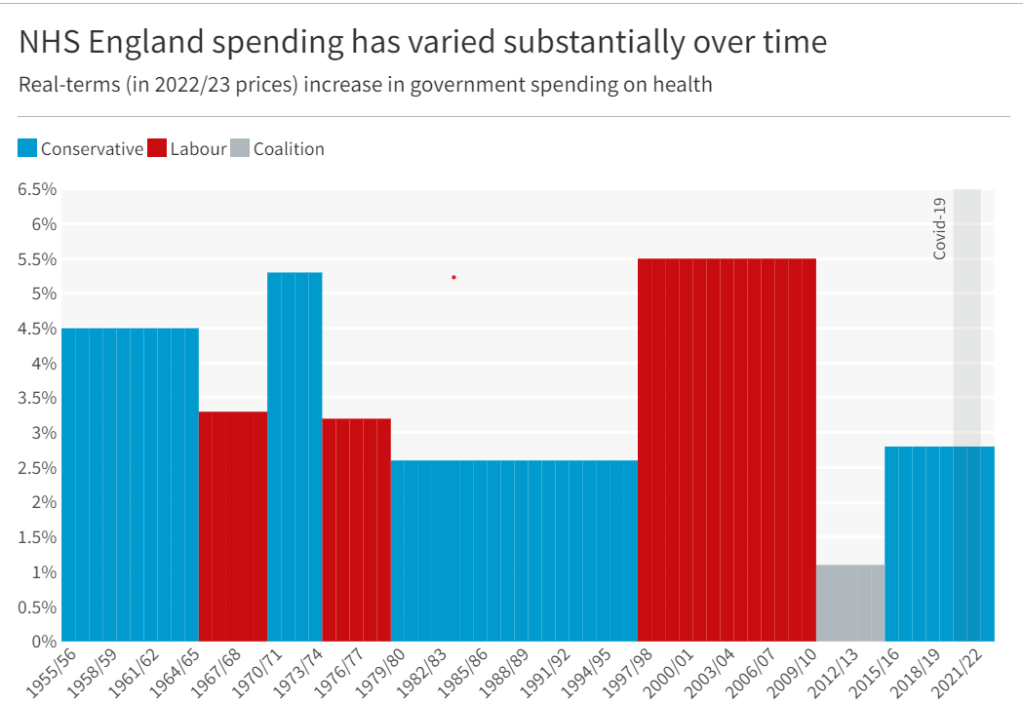
The NHS has been denied proper funding for more than a decade and has been repeatedly reorganised on different “business” models.
Our NHS hospitals and out-of-hospital services should run as a whole system service, not as competing businesses.
Healthcare provision is a major investment for any country. We say that investment should prioritise the health of the people and the workforce it employs not the quick buck for private companies.
The NHS was set up as a comprehensive public service, not a business opportunity, and for many years the NHS was the best in the world. In recent decades, for ideological reasons, many different pro-business, pro-privatisation models have been introduced at great cost. This coupled with inadequate funding and poor workforce planning has produced today’s multiple health crises.
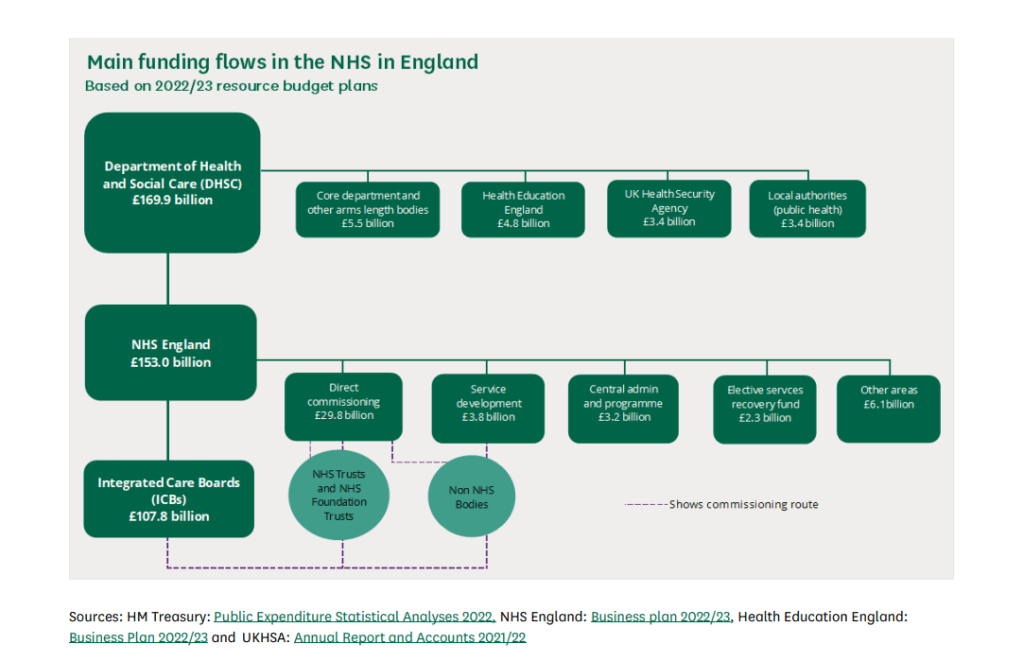
This diagram shows the flow of money into the NHS.
Strands in the NHS organisation structure (as produced by successive pro-privatisation governments).
A. The hospitals and out-of-hospital services like the GPs( primary care).
B. Big businesses including
- Those have contracts to run NHS services. There are many private companies operating publicly funded health care for profit. Some of these companies are causing serious system problems for funding and workforce training and problems for patients. There are serious concerns about some of these companies
- The financial consultants who are paid by the NHS to facilitate cuts or more privatisation.
- The political Advisors who advocate the privatisation model to the Government ( Samatha Jone has been removed from the Department of Health.
- The forty-two Integrated Care Boards across England
- Oversite frameworks like the CQC.
Hospitals and the ICB are in a tug of war for control of the public investment in healthcare. In 2024 the hospitals still function as individual businesses funded by the Government, some have comfortable bank balances, others repeatedly borrow at interest from the Government because they are structurally underfunded. Hospitals with big bank balances are not necessarily providing the best treatment and those having money problems can be providing good services. For more detail see this.
.In 2024 we have the ICB project. which splits the once national health service into 42 organisations modelled on the US ACO system.
This ICB model aims to create a regional organisation encompassing all government-funded healthcare in its region. Managing this crazy situation is National Health Service England (NHSE) and the Government. In our area, Cheshire and Merseyside, the ICB has problems.
“Board members will now be aware that NHS England has assessed the system as being at high risk of not delivering against the system financial plan submitted for the year ahead. Therefore, NHS England has mandated external support to undertake an urgent review. The ICB has engaged Price Waterhouse Cooper as the external support.”
This is not the first time Price Waterhouse Cooper has been called in about Cheshire and Merseyside. Within Cheshire and Merseyside, there are problems specific to Liverpool. These are problems of funding. There are three specialist hospitals in Liverpool that have been centrally funded, something the government intended to change. This is how Carnell Farrar, author of Liverpool Clinical Services Review reported the situation:
“The Cheshire & Merseyside ICS allocation per head to NHS organisations remains higher than all other core cities with the overall allocation due to decrease by c.£three hundred million over the coming years. Alongside this the new Specialised Commissioning allocation will mean that Cheshire and Merseyside will be allocated £50 million less income from specialised commissioning.”
We have seen denial of service, underfunding, the closure of beds and hospitals and the ICB system itself, all causing problems for patients. The work of the health service goes on, though diminished.
Each day a small army of 1.6 million people who make up the NHS staff go to work to provide healthcare and provide the daily miracles of skill, care, and kindness that we expect from our NHS. However, whilst millions are treated, millions of people do not get the care they need and we see many unnecessary deaths and suffering. But the big corporations still make huge profits from our NHS and thirst for more.
The NHS provides treatment for the vast majority of people in the UK though disgracefully, migrants are charged at 150% of the cost, or pay a surcharge for every member of the family, or are denied treatment.The huge scandal of denying treatment to NHS patients rumbles on. But this is what everyone could face if the privatisation project continues. England, Wales and Northern Ireland have slightly different NHS systems but all provide most treatments free at the point of need, funded by the Government.
It’s worth remembering that the US government spends more per person on healthcare, with worse outcomes, and most people pay huge insurance costs on top of Government spending. The US system is dreadful. Yet this is the model the previous government preferred, though it did not dare say so too loudly. Some Other wealthy countries either have a social insurance system or a mix of private and social insurance some use the original NHS model
“Each of the founding principles of the NHS is under attack: a universal, comprehensive service, publicly owned and accountable, funded through taxation and free at the point of use, with decisions on treatment taken on clinical grounds regardless of ability to pay.” (Tony O Sullivan, Keep our NHS Public).
Previous governments, including Labour Governments, have deeply damaged the NHS. What the last government did is qualitatively worse. This video from 2021 by Deborah Harrington from https://publicmatters.org.uk/ is a great description of what we face. What the new government will do remains to be seen, but those who value the work of the NHS must demand full restoration and repair.
Like many other public services, there are deep problems caused by underfunding, various forms of privatisation, and the selling off at knockdown prices of precious public assets. We campaign in the streets for our NHS, liaise with NHS workers, follow the open meetings, organise events and read and share documents. Government sources provide evidence of the situation. This is what the National Audit Office had to say, 23rd July 2024:
“The scale of challenge facing the NHS today and foreseeable in the years ahead is unprecedented.”
‘Deep financial deficits have now spread widely across the NHS and are having a substantial impact on patients. Some NHS trusts have been forced to reduce staffing or delay transformation plans that could give patients faster access and higher quality care when they need it.
The NAO report also says. “As they are statutorily required to do, NHS England and NHS systems have prioritised trying to live within their allocated funding. But, despite great in-year efforts to do so – some of which privilege the short term at the expense of the long term – an increasing number of NHS bodies have been unable to break even.”
The Integrated Care Board, the ICB set up over Cheshire and Merseyside, has financial problems. As a result, a firm called Price Waterhouse Cooper has been brought in to review their spending. Some of this spending is crucial to the safety of Liverpool Women’s Hospital. If Price Waterhouse Cooper disagrees with the ICB, then enforcers can be sent in to make the cuts.
Liverpool has more specialist hospitals than other cities. These hospitals do spectacular work way beyond the city boundaries. They are:
- Liverpool Heart and Chest Hospital NHS Foundation Trust (LHCH),
- The Clatterbridge Cancer Centre NHS Foundation Trust (CCC), and
- The Walton Centre NHS Foundation Trust (TWC).
Specialist hospitals are currently funded nationally, but plans are afoot to bring them into the ICB system. Our specialist hospitals exist because Liverpool is a core city, the largest in its region, surrounded by smaller towns and is a major port. This is not the first time concern has been raised about the future of the specialist hospitals .
Liverpool Women’s Hospital is partially funded by the specialist system, and mostly by the ICB.
Specialist hospitals are funded nationally. In our view, they should continue to be. This allows developments in treatment and expertise.
The new plan
All Liverpool Hospitals, except Alder Hey, will have major decisions made by the Adult Acute and Specialist Hospitals Joint Committee.
“The focus of the joint committee will be to establish the new governance arrangements, meeting in shadow form (i.e. no formal authority) in September 2024 and be in place formally (i.e. with authority to make decisions) by April 2025”.
The Chairs and Chief Executives of the five adult acute and specialist Trusts, outlined below, will sit on the joint committee:
- Liverpool Heart and Chest Hospital NHS Foundation Trust (LHCH),
- Liverpool University Hospitals NHS Foundation Trust (LUHFT),
- Liverpool Women’s NHS Foundation Trust (LWH),
- The Clatterbridge Cancer Centre NHS Foundation Trust (CCC), and
- The Walton Centre NHS Foundation Trust (TWC).
“This will enable more streamlined decision making and help to build upon existing collaboration with a specific requirement to collectively manage the financial position across the Trusts, deliver economies of scale and manage vacancy controls.” (Our emphasis. So it is about money and jobs).
The plans do not affect Mersey Care Foundation Trust. The proposals were published on the 29th of July. They are a follow-up to the Liverpool Clinical Services Review, produced by Carnall Farrar, one of the financial/business consultants who cost the NHS dear. Full details of the plans can be seen on our previous post.
What is NHS governance? “Governance” is defined by the NHS as
“the means by which provider boards direct and control their organisations so that decision-making is effective, risk is managed and the right outcomes are delivered.”
Trusts are already expected to cooperate with the local Integrated Care Board, the ICB.
“In addition to their existing duties to deliver safe, effective care and effective use of resources, the success of individual NHS trusts and foundation trusts will increasingly be judged against their contribution to the objectives of the ICS.”
The NHS currently operates within several models of organisational privatisation. Trusts were introduced in 1990. They were intended to make hospitals operate like businesses on the United States model. Then in the Health and Social Care (Community Health and Standards) Act 2003, Foundation Trusts were established. Then came the 2012 Act which brought in the commissioning of services to allow private companies to bid for NHS services. This legislation makes Trusts act like competing businesses. Then the 2022 Act brought in the ICBs which split the national NHS into forty-two different self-governing areas, modelled on the US Accountable care systems. The trusts still have legal rights but the ICB currently holds the money and with it the dominant power.
We call for a return to the original public service, not-for-profit-system, the Bevan model. The Bevan model was the most cost-efficient and the most equitable way of running healthcare and made the NHS for many years the best health service in the world. Look at where we are now!
For the patients, ‘system working’ (cooperation rather than competition between hospitals) is better than the ‘business’ model. For privatisers the ‘business’ model is more profitable and, long-term, will produce a system easier for to privatise and manage profitably.
The pandemic forced hospitals to function as a system not as competing entities and it worked! This is when CMAST mentioned above was set up.(See point 2.1 of this)
At the heart of this are the drive to cut NHS spending services, and workforce to make privatisation easier. The following are quotes from the Carnell Farrar report called Liverpool Clinical Services Review. There were fears for the specialist hospitals when the Carnell Farrar Review was published. Quite clearly funding is a key issue.
The misguided proposal to move Liverpool Women’s Hospital to the Royal has, fortunately, been withdrawn, as no funding was available. The idea of moving the Women’s Hospital to the Royal did not even get onto the ill-fated ‘forty new Hospitals’ promised by Boris Johnson.
We would rather the NHS management had focused on patient care and staff wellbeing. Below are direct quotes from the Carnall Farrar report which underline the key importance they give to finance.
1.Currently, NHS organisations in Liverpool are in financial deficit with an aggregated reported deficit position of £12.3 million at YTD (August 2022/23), which is expected to deteriorate further over the rest of the financial year.” (Carnell Farrell Report).
2. The Cheshire & Merseyside ICS allocation per head to NHS organisations remains higher than all other core cities with the overall allocation due to decrease by c.£three hundred million over the coming years. Alongside this the new Specialised Commissioning allocation will mean that Cheshire and Merseyside will be allocated £50 million less income from specialised commissioning. Local government in Liverpool and across Cheshire and Merseyside has also seen one of the largest decreases in real terms spending power since 2010 with a decrease of £700 per head of the population”. (Carnell Farrar Report).
3. “Liverpool has the greatest extent of deprivation in England as measured by the Index of Multiple Deprivation (IMD), with two in three people living in deprivation, and eight in every hundred people living in the most deprived one percent of the country. With respect to income, Liverpool is the most deprived local authority, and the most deprived with respect to employment and living environment.” (Carnell Farrar Report)
We oppose these plans because.
- The changes involve Liverpool Women’s Hospital and Liverpool’s Specialist Hospitals which are The Clatterbridge Centre, Liverpool Heart and Chest Hospital, and the Walton Centre. They each provide care beyond the city boundaries. But this decision system will focus on Liverpool.
- Liverpool Women’s Hospital works closely with other hospitals not in this network.
- Hospitals already collaborate across Cheshire and Merseyside. The Cheshire & Merseyside Acute & Specialist Trusts provider collaborative (CMAST) already exists to coordinate work across all the Acute and Specialist hospitals in Cheshire and Merseyside so cooperation and coordination are working before the proposals.
- These plans appear to be designed to restrict spending and we need more spending, more resources.
- These plans distance spending decisions from clinical and social necessity and put a greater distance between decision-making and the real life of the medics, hospitals, and patients.
- The plans do not include mental health provision, nor the out-of-hospital services provided by Mersey Care NHS Foundation Trust. Yet on Wirral, there is a drive to merge Wirral Community and Healthcare Trust with Arrowe Park Hospital, (Wirral University Teaching Hospital NHS Foundation Trust, WUTH). The plans affect Clatterbridge, who have a hospital on the Wirral working with WUFT and Wirral Community Health and Care Trust.
- The way money is allocated is as important as how much is allocated. We know how maternity has been treated in other hospitals
- The World Bank says “How service providers are paid matters as much as how much they are paid”.
- The further the money planning is away from the doctors, nurses, and midwives, the further it is from patients’ needs.
- The plans further the interests of those imposing the ICB system more deeply upon our NHS.
- The changes impact Liverpool Women’s Hospital. Liverpool Women’s Hospital serves way beyond Liverpool. It is a tertiary service taking cases across the area and beyond. It is a regional maternal medicine centre. We have a national maternity crisis. As the largest Maternity Hospital the problems with the Maternity tariff and the maternity insurance scheme impact LWH the most.Liverpool Women’s Hospital must focus on providing maternity care and women’s health. It needs cooperation with other hospitals, including but not only LUHFT. It must not have its financial decisions made by the much larger Liverpool University Hospitals Trust nor by the combined committee of the Liverpool Hospitals.
Maternity decisions should be made by people who know most about maternity. After all the reports on maternity problems, how can it now be relegated to a subdivision of a big hospital group?
Liverpool Women’s Hospital needs more midwives, a 24/7 consultant presence, better blood services and diagnostics and a medical team to tackle suddenly deteriorating patients. Above all, it does not need cuts.
However clever these management geeks are (they are not medics), they cannot solve the nationally caused problems faced by Liverpool Hospitals. They cannot turn on the taps for extra resources, but they can shut off vital money. It is gaslighting the city to pretend that new organisational layers can change the situation.
Every supporter of the NHS wants to see money going to front-line services, not to bureaucracy, not to outsourced privatised services. Everyone objects to the waste of money. These proposals do not address those issues. They create yet another layer of bureaucracy and financial control. Financial control often means implementing cuts.
Locally iaison between the hospitals already exists, through CMAST, Cheshire and Merseyside Acute and Specialist Trusts Collaborative, set up to good effect, during the pandemic, despite the privatisation and the business models.
These proposals will not go to public consultation. This is despite a written promise of consultation.
“Patients and public will be involved in the next stage, which is to develop proposals and to strengthen collaboration”.
Save Liverpool Women’s Hospital published these proposals as soon as we saw them. These plans include fundamental changes to Liverpool Women’s Hospital Board of Directors. The board is where long-term decisions are made about the hospital and where the public can catch a glimpse of what is happening. Liverpool Women’s Hospital will experience a two-fold impact, the joint board with LUHFT and the new super layer of management for Liverpool Hospitals.
“Shared Board of Directors for Liverpool University Hospitals NHS Foundation Trust and Liverpool Women’s NHS Foundation Trust”
Our health service is in crisis. It is inadequately funded and inadequately staffed and this situation causes preventable deaths, pain and suffering. For some people, this is death or pain and suffering during pregnancy and birth.
There is a national maternity crisis
This has been the subject of many authoritative reports that the last government failed to address. Another such report is due soon about scandals in Nottingham. Please see our other reports on this scandal. The House of Lords library provided a somewhat restrained summary of reports in January 2023. Maternity Service requires considerable extra funding to be truly safe and well-staffed.
There are unnecessary deaths, pain and suffering because of health service underfunding, understaffing and pro-business reorganisation. There are many millions of patients on long waiting lists for treatments, and crises in Accident and Emergency, mental health, maternity, dentistry and GP services.
The political intention has been to move our publicly funded and publicly provided healthcare to one which serves big business. We can hope Labour changes this, but Streeting is a fan of the private sector. This situation has been decades in the making since Thatcher. In this time fortunes have been made and hospitals have gone short.
The largest Tory Party donor who commented on wanting to shoot Diane Abbott MP, according to the Guardian, made his fortune from privatising services to the NHS.
“Hester, a businessman from West Yorkshire, runs a healthcare technology firm, the Phoenix Partnership (TPP), which has been paid more than £400m by the NHS and other government bodies since 2016, primarily to look after 60m UK medical records. He has profited from £135m of contracts with the Department of Health and Social Care (DHSC) in less than four years.”
No government has been fully open about supporting privatisation but privatise they did. Before any corporation would take over health care the government had to make it fit for profit. Beds and hospitals were closed. Hospital management was moved to an expensive business model, like the foundation trusts, where hospitals were expected to compete like businesses. This way, if a company took over, its responsibilities would be limited to the actual hospital and not the community. In 2015 a company, Circle, took over a major hospital. It was a disaster. It did not work, but the ongoing costs of the “business model” continue today.
A US model, called Accountable Care, (but then renamed in the UK as the Integrated Care System ), was introduced in the 2022 Health and Care Act. The Accountable Care model provides limited health care to the poor whilst giving great profits to the big corporations. You can read about it from the view of those who espouse this system here The focus is clearly on the providers capacity to make money.Many think tanks and commentators espoused the model yet now claim they are horrified at the state of the NHS.
The NHS now has inadequate money, fewer beds, insufficient doctors, nurses and midwives, and workforce planning has been appalling.
When NHS staff sat down to work out how to deliver services with inadequate money and inadequate staff, few if any intended what happened. And what did happen? The appalling planning for COVID, the destruction of mental health services, the damage to the GP service, the maternity crisis, huge waiting lists, and appalling situations in A and E. It is the cumulative effect of years and years of cuts, underfunding, corporate-style reorganisations and sheer wear and tear on the staff.
The UK has fewer hospital beds and fewer doctors per head of population than comparable European Countries. Our people have the worst access to healthcare in Europe. The Royal College of Nursing has declared a national health emergency because of the state of A&E. The answer is not to set up another layer of management.
Why are these plans confined to Liverpool? Why should a Liverpool-only committee make decisions about hospitals with a wider reach? Liverpool has an unusual number of specialist hospitals. They treat people from a wide area because they are specialists. They provide treatment that ordinary hospitals could not afford to fund or research. They are centres of excellence and research for staff. This new layer of management won’t provide extra expertise but it will create a situation where the
“focus of the joint committee will be on the management of capacity and demand, workforce challenges, collective financial management and governance arrangements for the five organisations”
It will also “Tackle challenges including the significant funding gap.”
Can this new committee tackle the workforce challenges for the most specialised fields in medicine? Solve them in one city? It can though restrict funding or divert funding. We say maternity and mental health have had enough of such restrictions already, do not let the other specialist hospitals go the same way.
The government wants (wanted?) everything under the auspices of the ICB. Then they could follow the US model and hand a whole ICB to a big US health corporation to manage for a lump sum. What the corporation does not spend becomes their profit, but that decision is theirs. You know, like the water companies and the railways?
The ICB provides the money. Why should there be another funding control except to restrict services just in Liverpool? Reading all the papers for board meetings for the Trust and for the ICB is challenging enough. Now these five members of this new committee are going to have to be familiar with all the specialist hospital issues, all the Maternity, Neonatal and Women’s health issues and the huge acute hospital and then make financial decisions, but only about Liverpool, although the hospitals deal way outside of the city boundaries.
We do not yet know what improvements in funding the current government will make, but the CEO of the ICB said at the July 2024 meeting that he did not expect significant changes.
Privatisation of public services has been an unmitigated disaster, from the excrement in the rivers and sea to, the utterly unreliable railways, and the neglect of children taken into care. Already there are huge differences in health services in different areas.
LUHFT ( The Royal Broadgreen and Aintree Hospitals) also provides specialist services way beyond Liverpool. For example, we know of people travelling to the St Paul’s Eye Hospital from as far away as Cornwall. The outpatient clinical space provision for St Pauls, before the new building, was frankly dreadful with cramped rooms for eye testing, difficult even for those with good sight to manage. How could a small specialist provision compete in a budgeting competition with immediate life-preserving services? These proposals would put the Specialist Hospitals in Liverpool under similar budget and organisational pressures to what St Pauls experienced in LUHFT.
There must be an end to cuts. An end to shaping health service systems on failed “business” models.
NHS services must be well-funded and well-staffed, with excellent laboratory backup, ambulance services, and effective care in the community. The fabric of the buildings must be adapted to demand to ensure safe environments for patients and staff. Working conditions, and the employment of fully qualified medical, midwifery and nursing staff as a priority. Workforce planning and staff retention must all be addressed.

Normally when hospitals cannot cope safely with the budget they are allocated, they apply for “drawdowns” from NHSE, England’s top NHS funding body. NHSE is currently refusing to give such monies to some hospitals. The Health Service Journal commented that “trusts are more likely to have their applications rejected or receive less than they asked for. Major trusts have warned of “slippage” in payments to suppliers.
“An email from NHSE’s finance team, seen by HSJ, said trusts applying for support need to provide assurances from their chair and CEO that they are on track with financial plan; have cash and cost controls in place; and confirm their workforce plans are on track.”
“Confirm their workforce plans are on track” does not mean they are to hire the doctors, nurses, and midwives they need, but the opposite. One whole ICB and their trusts have been sanctioned for recruiting too many staff.
We, with other campaigners across Merseyside, Cheshire,Lancashire and nationally, will keep up the fight to restore and repair the NHS. We will be lobbying Labour’s Conference, in Liverpool, in September. Please help by writing to your MP demanding the restoration and repair of the NHS.
Lets use this opportunity to make the case for a return to the Bevan Model of the NHS
More than 70,000 people have signed our petition to Save Liverpool Women’s Hospital online and on paper. The paper petitions represent 20,000 individual conversations about these issues.Please continue your suport.

Just to say that our NHS must be returned to its founding principles and that must include the demand for it to be PUBLICLY PROVIDED – by directly employed staff. That demand is too often omitted and it is critical if we want to keep our NHS public.
“Each of the founding principles of the NHS is under attack: a universal, comprehensive service, publicly owned and accountable, funded through taxation and free at the point of use, with decisions on treatment taken on clinical grounds regardless of ability to pay.” (Tony O Sullivan, Keep our NHS Public).
Yours
Sandra Ash
Sent from my Galaxy
LikeLike