These are notes from Lesley Mahmood and Sheila Altes, who gave the first responses to the proposals from the public presented at the ICB meeting on October 9th 2024. A more detailed response is being prepared. The ICB is the “Integrated Care Board” the big bosses of the NHS in Cheshire and Merseyside. You can find their papers here. The recording does not show the questions and contributions from the public but you can see some of those contributions on another post on this blog.
Points & questions for the ICB’s public meetings
(ALWAYS SAY YOU WANT YOUR COMMENTS NOTED IN DETAIL)
HOW & WHEN HAVE THESE PUBLIC MEETINGS BEEN ADVERTISED TO THE PUBLIC?
- “I want to question the whole basis of this meeting, this process and the nature of this ‘consultation.’
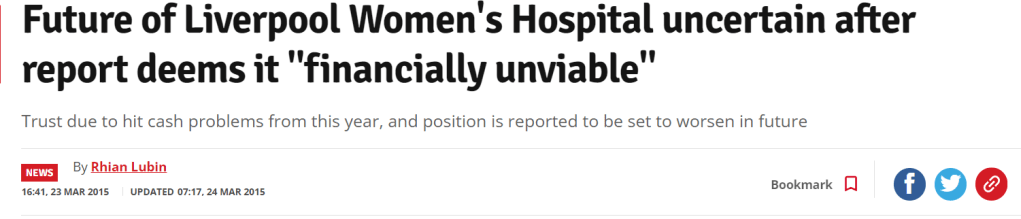
“Losing LWH at Crown St has been the ambition of NHS decision makers since March 2015 when the then chair of the CCG on Panorama stated Liverpool has too many hospitals & 1 has to go. The Echo had a story about it the day before. The day after the Panorama programme, the Echo’s lead story was the Women’s Hospital to close. That’s when our campaign started.
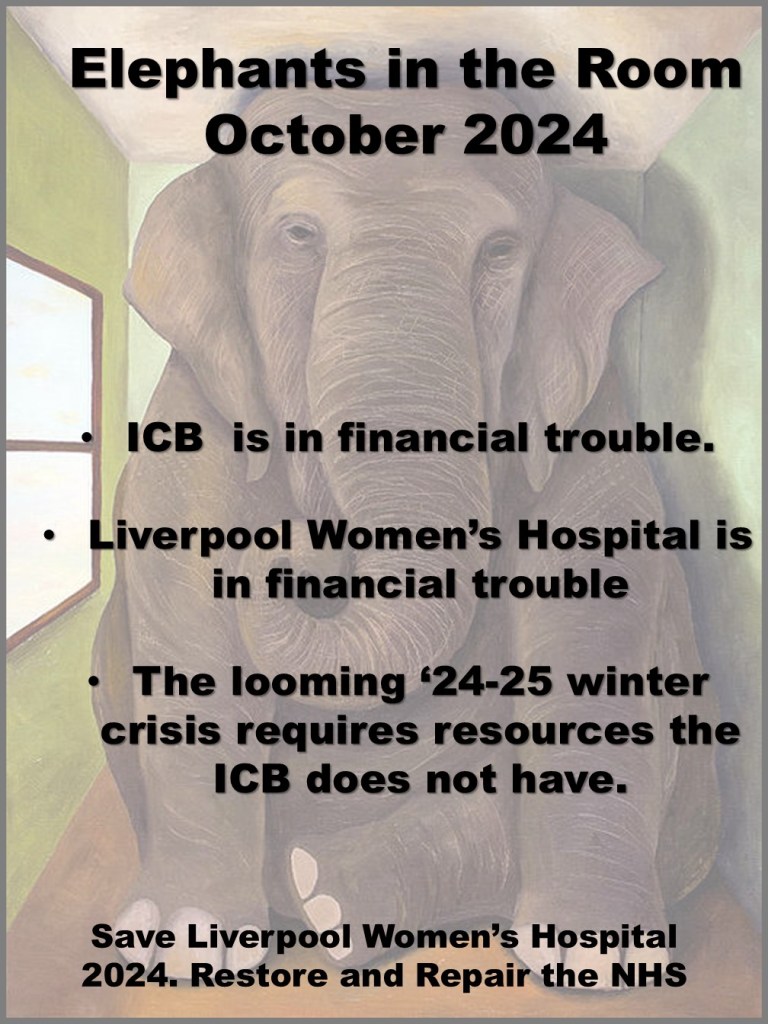
This 2024 ‘proposal’ is against the backdrop of closures of hospitals, A & Es, 1,000s of beds up & down the country. Some of these same decision makers told us that the Royal PFI/Carillion build with PFI & 300 fewer beds, a smaller A& E would meet the needs of Liverpool. Instead, we had massive debt, delays, A& E overwhelmed, 12-hour waits, and corridor care.
- Why avoid saying what’s to become of the Crown St site (on p.109 of the ICB document)?
In the last 12 months the ICB has indicated that £150m+ for an equivalent new build on the site of the old Royal is ‘unlikely’ ‘n the next 10 years. £150m is the deficit of the ICB. In Cheshire & Merseyside, Leighton is the only likely new hospital, which is falling in due to its crumbling concrete.
- So where’s the capital ( the money for buildings and costly equipment), or will we have 1 or 2 small Maternity wards tacked on somewhere? This will cause the ethos of the Women’s Hospital to be lost.
- What will replace LWH at Crown St? It’s not good enough to say it will be used by the NHS; who will provide them, private companies like Spire/ Spa Medica? Under the Naylor Report, surplus’ and not fit for purpose NHS buildings or land is to go up for sale. We have been told by staff in Spire that Spire is very interested in Crown St.
Why should a £15m new neonatal unit & a new scanning unit of several £m be scrapped?
Women in Liverpool 8 & beyond regard LWH at Crown St as a safe space, a green space (good for recovery & mental health), a low rise, easy to get into in an emergency, especially valued by the L8 community, who regarded the LWH being developed at Crown St as part of Project Rosemary after the Toxteth Uprising of 1981 as some compensation. The wife of the Dean of Liverpool signing our petition recently said -he was 1 of the people responsible for Project Rosemary. The LWH is also valued by the other 75,000 people who have signed our petition.
- There’s no mention of the positive impact of LWH being based at Crown St. On p.107, it is claimed that Crown St means worse gender inequality. Where is the evidence for this? On p.63, for instance, the maternal mortality is in line with national data and where is the equality impact assessment referred to on p.110?
- The ICB document talks about 5 risks at Crown St, I want to question these.
RISK 1. Acutely deteriorating women cannot be managed onsite at Crown Street reliably, which has resulted in adverse consequences and harm.
( We know this experience can be horrible for the women involved)
The paper cites the cause as a lack of onsite services and specialist staff, e.g. critical care, medical and surgical specialities and 24/7 blood transfusion labs. At present, there is not a critical care unit (CCU) available at LWH, but there is a high dependency unit (HDU) at Crown Street and staff at the gynaecology HDU have undertaken training for critical care.
- The Core Standards for Intensive Care Units (2013) state that it is preferable to have an intensive care unit on site, but units without such a provision must have an arrangement with a level 3 CCU and a policy for the safe transfer of patients when required. LWH has such an arrangement with the Royal Liverpool University Hospital (RLUH) which is situated 1.3 miles away.
- A lack of medical and surgical specialities was also cited. A Medical Emergency Care Team is being recruited to enable optimal care and transfers if necessary. LWH is also participating in the “deteriorating patient collaborative” to improve earlier recognition of clinical deterioration. There are clinical pathways in place for the acutely unwell/critically ill pregnant or recently pregnant woman. Women with complex needs are seen at specialist clinics, where a consultant obstetrician and consultant in the relevant specialism will plan the treatment necessary to ensure optimal care. LWH is the recognised provider of high-risk Maternity care and complex gynaecology procedures in Cheshire and Merseyside. Emergencies will inevitably occur, and a transfer to a CCU will be needed. Inter hospital transfers of critically ill adults take place frequently, it is estimated that 10,000 of such transfers take place annually in the UK (BJN 22/04/21).
- A 24/7 Blood Transfusion lab is to be developed at the Crown Street site. As well as the extension of some laboratory services.
- Given all of these developments and the small number of patients being transferred to CCU (see page 46 of the Case for Change), why does the ICB consider co-location necessary, especially in a time of financial restraint?

RISK 2: When presenting at other acute sites (e.g. A&E), being taken to other acute sites by ambulance or being treated for conditions unrelated to their pregnancy or gynaecological condition on other sites, women do not receive the holistic care they need.
Board papers state that the risk is caused by a lack of women’s services and specialist staff at other sites in Liverpool. However, it is difficult to see how re-location would solve this if LWH is re-located to the RLUH; women are still likely to turn up at the Aintree site and vice versa.


- Is the ICB looking at Maternity and gynaecology services at 2 different sites? How will this fit with LWH as a Maternal Medicine Centre (MMC)?
- LWH has its own Emergency Department with much shorter waits than the Royal/Aintree A&Es, if LWH is moved, will its Emergency Department close and women have to queue up in the general A&Es?
- This dispersal of services would not fit with the ethos of a specialist hospital for women, and that surely would be a gender inequality, as women’s health differs from that of men in many unique ways. It is influenced by biology and conditions such as poverty, employment and family responsibilities. Women’s reproductive and sexual health have a distinct difference compared to men’s health. (Cardiovascular disease, common to men and women, can lead to pre-eclampsia in a pregnant woman. Sexually transmitted infections can cause such outcomes as stillbirth or neonatal death. Other issues impacting women’s health include unplanned pregnancy, non-consensual sexual activity, domestic violence and female genital mutilation). Centres of excellence in women’s health, such as LWH, can advance research and large-scale clinical trials to address these issues, but the dispersal of services cannot.
RISK 3: Risk 3: Failure to meet service specifications and clinical quality standards in the medium term could result in a loss of some women’s services from Liverpool.
- Maternal Medical Centres (MMC) are responsible for ensuring that all women on the network’s footprint with significant medical problems will receive timely specialist care and advice before, during, and after pregnancy. LWH has been selected as one of 3 MMCs within the North West, along with St. Mary’s Hospital in Manchester and the Royal Preston Hospital in Lancashire. The model of care ensures that the highest risk and most complex women will have most of their care delivered by the MMC.
- No hospital in the UK is equipped to deal with every eventuality. Therefore, it is inevitable that patients sometimes have to travel outside their area.
- At present, women with complex congenital heart conditions are sometimes treated in Manchester. The RLUH cannot deal with some complex bowel surgery, and patients sometimes have to travel to the Christie Hospital also in Manchester. Yet, there are no questions about relocating the Royal, so why the Women’s Hospital?
Risk 4: Recruitment and retention difficulties in key clinical specialities are exacerbated by the current configuration of adult and women’s services in Liverpool.
- Recruitment and retention of staff is a national crisis in the NHS as a whole and not just in Maternity services.
- There has been a 9-year threat to reconfigure services at LWH, which may have hurt recruitment.
- As a teaching hospital, LWH is a centre of excellence in the provision of undergraduate and postgraduate medical education and training. LWH has a highly active multidisciplinary research programme that includes research into Maternity studies, gynaecology studies, fertility studies, genetics, oncology and neonatal studies.
- The claim that the difficulties in recruitment are caused by an inability to provide comprehensive multidisciplinary team working and training on acute sites makes Liverpool Women’s Hospital a less attractive place to work is hard to believe. We favour joint appointments and joint working to provide comprehensive training and development opportunities.
- Governments have deliberately reorganised and underfunded the NHS. There is a national Maternity crisis. Maternity nationally has historically been underfunded through the Maternity tariff. This affects LWH particularly. So, fund it, don’t lose it!
RISK 5: Women receiving care from hospital services, their families and the staff delivering care may be more at risk of psychological harm due to the current configuration of services.
- In a time of increased misogyny, violence towards women and austerity policies that disproportionately affect women, LWH is seen by all women of all ethnicities, as a safe place for women.
- For the last 14 years, NHS staff have been underpaid, overworked, and undervalued, conditions exacerbated by the pandemic that still continue. The Ockenden review highlighted these issues throughout the country, so psychological problems are not exclusive to the Women’s Hospital.
- In a recent staff survey for the LWH Board, 49% of staff feeling negative about their work said they felt overworked. (p.24 People Pulse report, LWH Board papers 10.10.24)
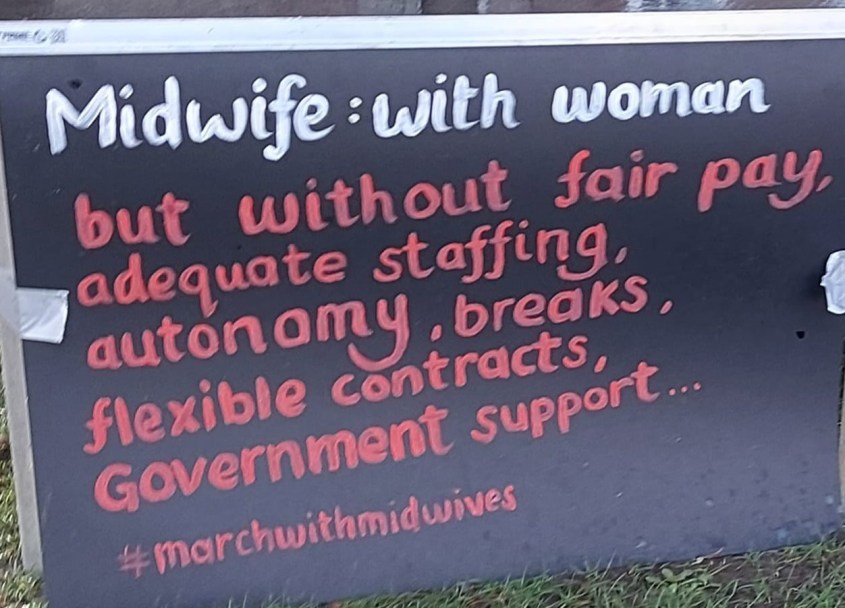
- Ockenden called for more staff, more midwives, and more Maternity funding. We need more midwives & we need to keep experienced midwives to support newer midwives.