March for Liverpool Women’s hospital 2018 4
” We must save it”. Save Liverpool Women’s Hospital campaign has spoken with over 4,000 people this summer of campaigning.
 Some people have asked us questions about how and why the “relocation” of the hospital is being proposed. This then is an attempt to answer some of those questions.
Some people have asked us questions about how and why the “relocation” of the hospital is being proposed. This then is an attempt to answer some of those questions.
In a cash strapped NHS, should £140 million pounds be spent “relocating” a perfectly good hospital less than a mile down the road?
Should we be suspicious if this is in an area being gentrified?
Should a modern low-rise hospital in landscaped grounds, set back from the traffic, be rep
laced by a high-rise in the middle of some of the densest traffic in the city?
Should such a move be pushed on the false basis that the move would save money?
Should we take the risk of losing an exceptional hospital in a time and an environment so hostile to the NHS, in a situation of crisis, spring, summer, autumn and w
inter in the NHS? Or should we say, like the Merseyside Pensioners Association say “What we have we hold!”
 The Liverpool Women’s Hospital is explicitly safe. The CQC report indicates this and all sources confirm this. If you want more detail please see here
The Liverpool Women’s Hospital is explicitly safe. The CQC report indicates this and all sources confirm this. If you want more detail please see here
The day-to-day problems of funding for Liverpool Women’s Hospital come from the underfunding of the NHS nationally, and from an inadequate maternity tariff. The idea that savings from sharing some services at the Royal can bridge that gap or even pay for the £140 million move is not credible. Recruitment at Liverpool Women’s Hospital is traditionally good because it is a world-famous hospital.
The main decisions about the Liverpool Women’s Hospital are, officially, made by the Board of Directors of the Liverpool Women’s Hospital and the Liverpool Clinical Commissioning Group. Liverpool City Council Health and Wellbeing board has a say too. Liverpool City Council is working with other organisations as part of plans to integrate health and social care. This larger group could have a say too, though not immediately.
Just to be clear, it’s not the doctors, midwives and neo natal nurses making the decisions. Not here, not anywhere in the NHS. There are few doctors on the board. Clinical directors do not often attend the board meetings. Relationships between the hospital upper management and the staff are not always sweetness and light as the annual NHS survey indicates.
Liverpool Women’s Hospital has a regional role too. It provides services for women, babies and some men from across the region, into North Wales, and the Isle of Man. These services include the treatment of complex cases. Plans for the future of this hospital go to the other Merseyside Councils, in a joint committee for approval too.
 Liverpool Women’s hospital’s role as a neonatal centre has just been further developed by a grant of £15m funding to improve and upgrade its existing Neonatal Unit. Th re have been other improvements too in Outpatients department, and in the refurbished Gynaecology Unit.
Liverpool Women’s hospital’s role as a neonatal centre has just been further developed by a grant of £15m funding to improve and upgrade its existing Neonatal Unit. Th re have been other improvements too in Outpatients department, and in the refurbished Gynaecology Unit.
Merseyside and Cheshire have an Sustainability and Transformation Plan area that is supposed to plan NHS provision in its area (and make further huge cuts of almost £1billion across the area), and parallel to that is the Women and Children’s Vanguard , which nationally answers to the Maternity Review
The Maternity Review is pro privatisation, both in the use of for profit providers, encouraging dispersing services from hospitals and in developing costing mechanisms through the personalised budget system.The safety and effectiveness of the maternity review is called into question here .
Already many women have been charged for NHS maternity care based on their migration status even if they are living and working here, or if they are UK citizens returning here the costs are enormous.
T he pressure to use private providers, (one such organisation has been placed on enhanced surveillance) and to encourage home births are also part of the maternity review. Maternity care should respect the mother’s wishes AND must always be safe for mother and baby. Some of the ideas that over promoted natural child-birth by criticising provision that used interventions in childbirth, have already been rolled back since our campaign started in 2015. Home births for those who want them and for those for whom it is safe, are great, but the vast majority of women choose the safety of the hospital.
he pressure to use private providers, (one such organisation has been placed on enhanced surveillance) and to encourage home births are also part of the maternity review. Maternity care should respect the mother’s wishes AND must always be safe for mother and baby. Some of the ideas that over promoted natural child-birth by criticising provision that used interventions in childbirth, have already been rolled back since our campaign started in 2015. Home births for those who want them and for those for whom it is safe, are great, but the vast majority of women choose the safety of the hospital.
Many NHS budget crises, including that in Liverpool Women’s Hospital are temporarily supported by what’s called Transformation or Sustainability funds; it’s not quite the same thing as the STP areas, but came in at about the same time.
The NHS nationally must be formally consulted too about major expenditure. The NHS national structure is s complex. There is a set of slides available here but there have been changes since this was written. The laws changed in 2013 with the health and social care act and another major change is under way at present.
Consultations with the national NHS bodies are detailed and the ones about the Liverpool Women’s Hospital have been back and forth a few times, according to reports to the board.
 Two streams of money go into the NHS, Revenue for day-to-day spending and capital for major projects. Capital funding is the permission to spend money on long-term projects like new builds, refurbishment, major equipment and the like. NHS capital funding is not doing very well, falling for three years in a row ( Capital spending does well for the big corporations making a packet from it)
Two streams of money go into the NHS, Revenue for day-to-day spending and capital for major projects. Capital funding is the permission to spend money on long-term projects like new builds, refurbishment, major equipment and the like. NHS capital funding is not doing very well, falling for three years in a row ( Capital spending does well for the big corporations making a packet from it)
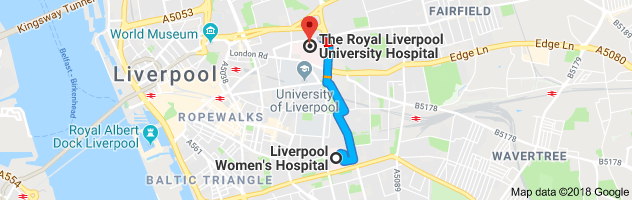
A bid for capital funding needs to be made if the current plans for a “relocation” are to go ahead. The plan is to relocate Liverpool Women’s Hospital to the traffic island that is the new Royal site (Prescot St, Liverpool L7 8XP)
There is a problem that this, and the last, government wanted to keep big capital expenditure off their books. They falsely believe that borrowing for investment can lead to a financial crisis. Its plain nonsense, details here. Keeping big borrowing off the government books has given big corporations like Carillon the chance to make a fortune from Private Finance Initiative which have resulted in hugely expensive and often badly built hospitals and schools.
At present there is no published source for the money for the Liverpool Women’s Hospital Boards plans. Unless there is a major turn in Government policy the money for this relocation will come via PFI, or possibly a loan from Liverpool City Council,. who will themselves have to borrow the money. Liverpool city council has its own major financial problem thanks to appalling austerity cuts from this government.
 The abominable chaos that is the new Royal Liverpool build has to be sorted out at huge cost. The full cost is not yet known, nor who will bear that cost. Never the less we are expected to believe that this will have no impact on decisions about money to relocate Liverpool Women’s hospital at the projected cost of over £140million on the same site.
The abominable chaos that is the new Royal Liverpool build has to be sorted out at huge cost. The full cost is not yet known, nor who will bear that cost. Never the less we are expected to believe that this will have no impact on decisions about money to relocate Liverpool Women’s hospital at the projected cost of over £140million on the same site.
Policy issues are decided by government and by their appointees in the NHS, like Simon Steven.They are not the polices the people of liverpool generally support.
There are two professional disciplines involved in planning health care, one is medicine which is the patient facing care and the other is health economics. The health economics planning in the last ten years have been disastrous, and politically committed to the privatisation and US model.
Lets look as some of the errors this group have made
1. Hospital beds numbers have been closed down but are desperately needed.
2. The internal market introduced to make hospitals compete has been an expensive disaster.
3. Staff shortages. Insufficient doctors , nurses and midwives have been trained. This is a planning failure, not an accident
4. Bursaries have been stopped.
7. Outsourcing and commissioning private companies to deliver health care has been costly and ineffective. Private companies made £831m profit from such contracts.
Doctors Nurses and Midwives and the related professions correctly want to be able to co-operate across hospitals, across disciplines. What stops this is not the physical placement of the buildings, but the trust system and the internal market.
Broadgreen Hospital and the Royal constitute one trust and are talking of merging also with Aintree . These buildings are much further apart than Liverpool Women’s Hospital and The Royal Liverpool University Hospital. Talk of an “isolated site” in this situation is a nonsense.
Long term intensive care at level 3 is not available at Liverpool Women’s Hospital. Short term intensive care is available at LWH. Those who need long-term intensive care are transferred to the Royal. 6 minutes away, by ambulance. This is less time than it would take to push a patient through areas of some hospitals. It would cost a lot less than £140m to upgrade the service at LWH. Services which do cause problems are ones that the hospitals already share.
 Our campaign is very realistic about the strengths and weaknesses of Liverpool Women’s Hospital. We heard some breath-taking stories whilst we were campaigning, some of wonder at lives started and others saved and some less happy. We met so many happy babies, and lovely children born there. Some of you we spoke to might like to share your stories on our Facebook page or in reply to this.
Our campaign is very realistic about the strengths and weaknesses of Liverpool Women’s Hospital. We heard some breath-taking stories whilst we were campaigning, some of wonder at lives started and others saved and some less happy. We met so many happy babies, and lovely children born there. Some of you we spoke to might like to share your stories on our Facebook page or in reply to this.
More than 40,00 people have voiced their opposition to these proposals. Our campaign wants
- to keep our hospital focussing on women’s health, the average British woman has 19 years of ill health.
- to keep maternity provision safe and away from traffic fumes and particulates
- to obtain better funding for the NHS and especially for maternity.
- to pay staff well, recruit, train and retain more staff.
- to oppose privatisation and PF.
- to end the rationing of care.
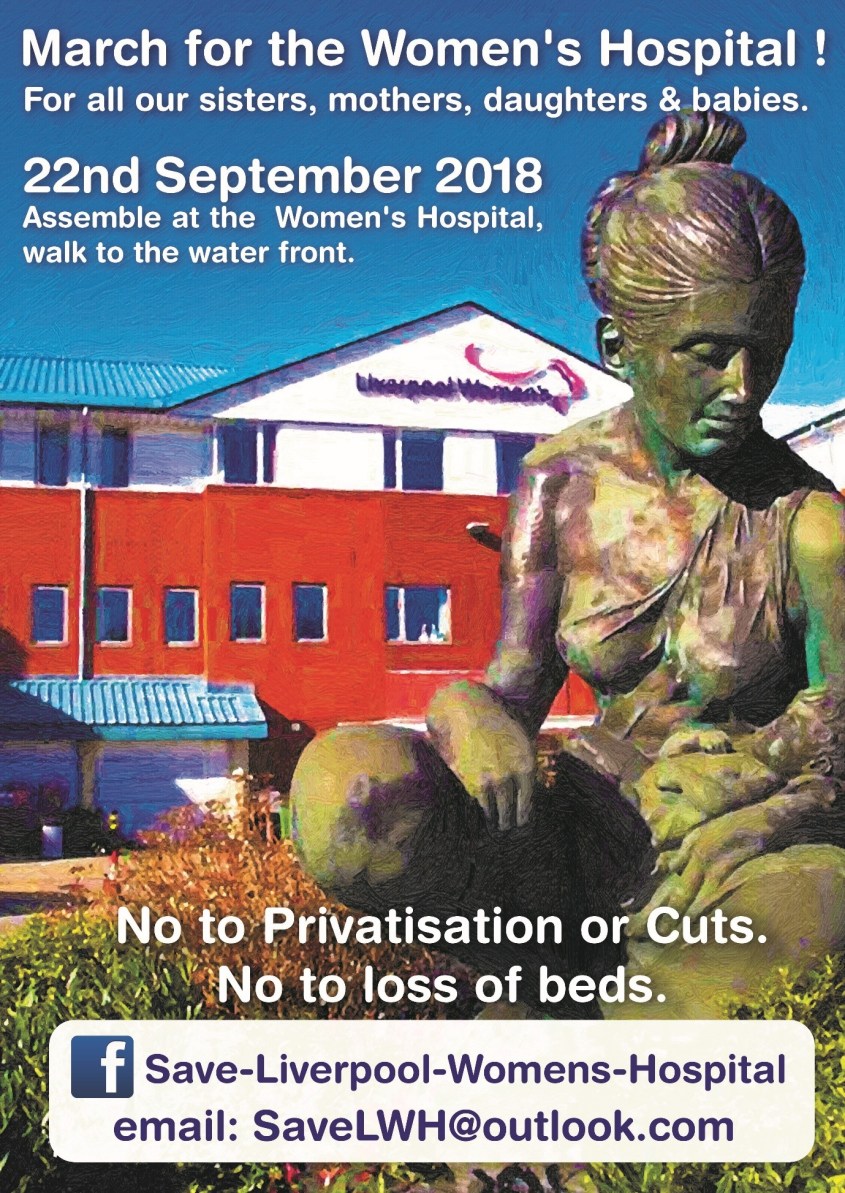 Please march with us on September 22nd 2018 at 12 noon to Save Liverpool Women’s Hospital and Save the NHS. This is the next stage in our campaign Fight like your grandmother did to get the NHS
Please march with us on September 22nd 2018 at 12 noon to Save Liverpool Women’s Hospital and Save the NHS. This is the next stage in our campaign Fight like your grandmother did to get the NHS

