January 2025

“Save the Liverpool Women’s Hospital. No closure. No privatisation. No cuts. No merger. Reorganise the funding structures, not the hospital. Our babies and mothers, our sick women, deserve the very best”. We repeat this as the NHS governing body in Cheshire and Merseyside presents “new” proposals for Liverpool Women’s Hospital. We have more than eighty thousand people supporting our position on our petitions, online and on paper. The paper petition represents tens of thousands of face to face discussion with the public.

Our options for Liverpool Women’s Hospital
Liverpool Women’s Hospital is in the eye of two storms: the NHS as a whole and the National Maternity Crisis. We refer to corridor care, recurring winter crises, long waiting lists, too few doctors and too few beds, and significant waste from privatisation and a competitive rather than cooperative structure between hospitals. We also refer to the Maternity crisis, where yet another enquiry is underway and where the outcomes for women have gone back 20 years.
We demand that the Government and our local MPs restore, repair, and rebuild the NHS.
Amid these storms, options for Liverpool Women’s Hospital’s future were discussed at the ICB on 29th January 2026. They include options that have been presented before and met with huge opposition, as demonstrated by the popularity of our petition and demonstrations. There is no national background given on the NHS’s huge financial problems due to underfunding, nor on the national Maternity crisis. The ICB papers can be found here.
We demand candour about the financial pressure that led to the ICB proposals. We demand candour about the financial pressures that have led to so many Maternity units closing or being merged into worse facilities, including acute hospitals, further from the women they serve.
Option 6 in the ICB papers proposes moving some services to smaller rooms in the Royal, rather than keeping the Maternity Gynaecology, the NICU, and other services at the Crown Street site. “This would involve compromises and standard room sizes“, including for neonatal services. This is unacceptable, especially as Liverpool Women’s have been celebrating how good the new NICU (Neonatal Intensive Care Unit) at Crown Street is. As one staff member from the Royal said with heated emphasis, “There is no room for the Royal in the Royal”.
We do not oppose certain complex operations taking place at Liverpool Royal Hospital. Such cooperation should have happened years ago.
We presented a detailed, referenced document to the ICB on the future of Liverpool Women’s Hospital, but it does not appear to have been used. Our offers to meet with the working party have not been accepted, and the significant opposition has not been addressed in their published documents.
We are concerned about some of the wording in these proposals. For example, in the Equalities Impact Assessment (page 2, para 5), it states that, across all options, the future model “is expected to include increased clinical presence across acute sites.”
That phrase ‘expected‘ is worrying, as it seems to offer no guarantee that clinical support will be increased or even maintained, whatever the configuration. Yet poor maternity staffing acuity has been at the heart of Ockenden’s findings, the Amos interim review, and RCM’s recent criticisms of understaffing.
Also, on the consultation timelines being proposed before proceeding to a business case. Six weeks is being recommended. Given the report earlier concedes that the options, including the preferred option, will mean considerable changes to patient care, are complex in nature and have aroused widespread public and political interest, the consultation period proposed looks far too short and a longer period say 12 weeks might allow for example the various local councils scrutiny committees and public health to review (and also allow more interrogation of the options)

The ICB has a huge financial problem. Although on a smaller scale, Liverpool Women’s Hospital also faces major financial problems because it relies on the Maternity Tariff, which is nationally inadequate. Moving the hospital would not tackle this problem.
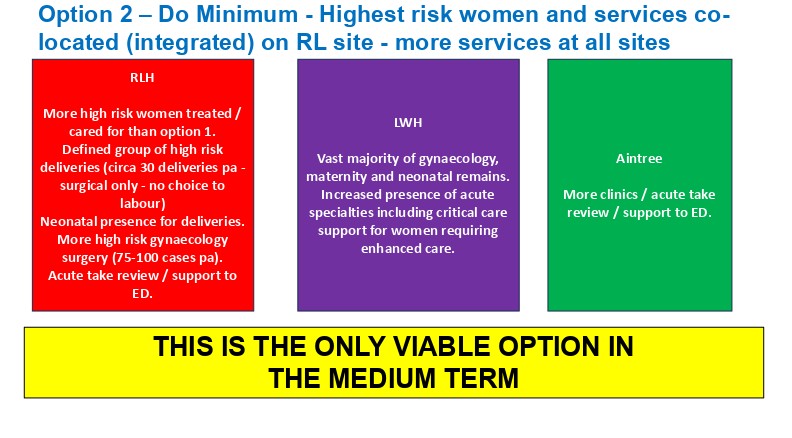
Two main options were presented at the meeting for the future of Liverpool Women’s Hospital: a short-term and a long-term plan. They are both based on the idea of moving Liverpool Women’s Hospital long-term into the Royal. The short-term option, option 2, involves most of the services remaining at Liverpool Women’s Hospital, but about thirty high-risk surgical deliveries are planned at the Royal, and about seventy-five gynaecological operations are also scheduled there. Many of these ideas are good, but not with Liverpool Women’s losing management of them and not as a step towards putting all the services into the Liverpool Royal.
This is the commentary from the board papers on option 2
Option 2 – Key Service Details
6 bedded enhanced care unit, with improved facilities and accommodation, on the LWH site – cohorting 4 existing beds (2 maternity, 2 gynaecology) and 2 additional beds to accommodate future demand. ( our response;”Good if the finances are made available)
Appropriate accommodation and capacity (beds/theatres / critical care) provided at the RLH site for additionalgynaecology operations and high-risk births. This would include additional neonatal support for births (staff, kit, transport). Our response. Why can this additional capacity not be provided at Liverpool Women’s Hospital, where mothers and babies can be together and where the whole expert NICU staff are based?
Greater investment in obstetric physician time (from 1 day to 5 days p.w.)( our response: “Good if the finances are made available)
Investment in visiting AHPs and therapist staff not currently provided for at LWH (e.g. OT, nutrition, SALT).( our response: “Good if the finances are made available)
Investment in adult acute medical time to manage the required input to LWH (e.g. colorectal, urology, cardiology).( our response;”Good if the finances are made available)
Consultants of the day (one for gynaecology and one for maternity) and increased consultants on call (gynaecology, maternity and neonatology) to enable cover at non-LWH sites (including attending EDs / completing ward rounds).( our response: “Good if the finances are made available)
Increase outreach midwifery to 24/7 – for visiting non-LWH sites( our response: “Good, but only if the additional finances and staffing are made available).
New role for outreach specialist gynaecology – for non-LWH sites – in particular for older women post op. ( our reponse is that this needs more explanation. We do not wantto see older women getting a second-class service.
Dedicated ambulance resource for inter-site transfers. (Our response: We have suggested this in the past.)
The second set of options (called option 6 )involves moving most of the Women’s services to the Royal. Or, and they say this is very unlikely, building a new building at the Royal. They are not consulting on these options. They are consulting on option 2 as a stopgap. However, they said at the meeting, there would be “No stepping back from the long-term support for option 6 “( moving into the Royal)
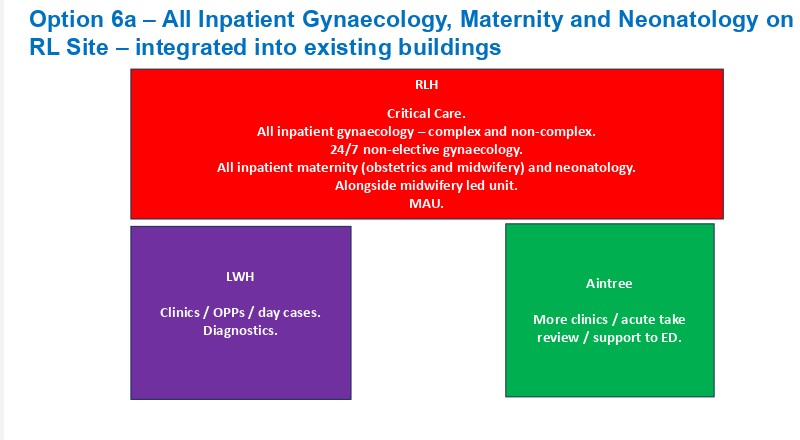
Worse physical conditions!
The plans on Page 36 of the Cheshire and Merseyside ICB paper, dated 29th January 2026, make it clear that the physical environment will be worse than the national standard and certainly worse than at the existing Crown Street site.
“The test-to-fit exercise for option 6a confirms that all major functional elements can be accommodated withinthe RLH estates envelope with some compromises.
Existing derogations within the RLH would need to be accepted, e.g. there would be some compromises on standard room sizes (all single rooms are approximately 4sq.m. under sized) and there is no isolation provision on a typical ward.
For neonatal services:
• A typical IC / HD cot space allowance is sized at 20.q.m. The test to fit exercise indicates a range of around 12q.m. to 15sq.m.
• A typical special care cot space is around 11.5sq.m with a test to fit range of 8sq.m. to 11sq.m.
The existing size and shape of the Royal Liverpool Hospital building would mean some services may need to be configured differently and/or require different staffing models e.g. maternity wards.
Structural and MEP (Mechanical, Electrical and Public Health) constraints – e.g. birthing pools, theatre ventilation and drainage on Level 9 would require further investigation in subsequent design stages.
Detailed design work would be required with clinical teams in order to test this option further.
Liverpool Women’s Hospital is not more dangerous than other Maternity services, far from it. Behind each option is an implicit implication that Liverpool Women’s Hospital is somehow dangerous. In another item in the ICB reports, the Local Maternity System reported that Cheshire and Merseyside Maternity had better outcomes than two neighbouring ICBs. Liverpool Women’s Hospital is the largest Maternity provider in Cheshire and Merseyside, so the “dangers” appear to be limited.
Liverpool Women’s Hospital does need improvement, as does most of the NHS, after years of cuts. However, last year the Care Quality Commission, which inspects all hospitals, rated Liverpool Women’s Hospital “Good” across all five criteria: Safe, Effective, Caring, Responsive, and Well-led. This is at a time when the Care Quality Commission reported that “ Under our assessment framework introduced in 2024, we have published the findings of inspections for fifteen maternity services. Of these, two-thirds of services (66.7%) have been rated as inadequate or require improvement, with a third (33.3%) rated as good. No services have been rated as outstanding.”
Fourteen hospital trusts are being investigated for Maternity safety failings. Liverpool Women’s Hospital is not one of them. MBRRACE organises national surveillance and investigates the deaths of all women and babies who die during pregnancy in the UK, so each woman’s death is investigated nationally. We can find no mention of dangers from a separate site.
NHS Hospitals should work together as a system. The 2012 Act was described by Lord Darzi as “a calamity without international precedent” and a “disastrous” piece of legislation. The 2012 and the 2022 legislation sought to treat hospitals as separate competing companies. It was a disaster. We support inter-hospital cooperation.
Transfers between Hospitals are routine. Too few women become extremely ill at Liverpool Women’s to justify a level 3 intensive care unit, so very occasionally an extremely sick woman needs to be transferred. This is not a pleasant experience. However, no evidence was presented at the ICB meeting that more women die at Liverpool Women’s Hospital than at other Maternity hospitals, nor that they die because of being moved to the Royal, one mile away. One good suggestion was to establish a dedicated Ambulance service for transfers. Other hospitals in the Liverpool Group are much farther apart, yet they transfer patients between them. There is no suggestion that those hospitals should be moved.
Please help us to continue the fight to save Liverpool Women’s Hospital, to repair the national Maternity service and to fight to Repair, Restore and Rebuild the NHS. Please help us.
Our alternative to the Options presented by the ICB.

- Keep Maternity, Gynaecology, the NICU, Genetics and Research, all the existing services, at Liverpool Women’s Hospital, at the Crown Street site. The experience of placing Maternity services in large acute hospitals has not been good. There is little evidence to support the practice, and much to disprove it, as shown in the current Maternity crisis and investigations into Maternity failures. Preserve Liverpool Women’s Hospital as a women’s service, for all our mothers, sisters, daughters, friends and lovers and every baby.
- Improve birth outcomes and experiences for women and babies.
- Improve post-natal care for all women.
- Improve the national funding structure for Maternity.
- Improve cooperation and joint working with other hospitals and other NHS providers.
- Improve funding to allow many more midwives.
- Improve funding to allow more medical staff for deteriorating patients.
- Employ more Gynaecology staff to address the long waiting lists, recognising this is a national and local issue. Stop outsourcing to cosmetic surgery hospitals.
- Provide free parking for staff.
- Provide a dedicated ambulance service between Liverpool hospitals to take pressure off the emergency service, so badly hit in the (entirely avoidable) winter crisis.
- End outsourcing to private health companies.

The press statement we sent out.
“At their meeting this Thursday, the ICB Board approved a report outlining several options for Liverpool Women’s Hospital, all of which will move services away from the hospital at the Crown St site.
The ICB favoured option is 2, which sets up some ‘high risk’ Maternity and gynaecological provision in the Royal.
Campaigners asked the ICB formal questions submitted before the meeting. Against earlier practice, they declined to let questioners speak.
Why has there been so much waiting and suffering in A and E, so much corridor care, so many long trolley waits for admission to the wards, all of which costs lives, pain and indignity at the Royal, if there is spare capacity in the hospital available for Maternity, neonatal, and gynaecology on Level 9?
Why is there no mention of the opposition to these plans from the community, trade unions, and campaign groups? We refer to this comment from the ICB’s own papers, 24 07 25.
Why are the financial (both capital and revenue problems) of LWH based on the issues with the Maternity Tariff, not mentioned in these options? How will any of this help the hospital’s financial problems? Will these options not increase the administrative load? Why are there no costings, and why is there no mention of the likelihood of gaining significant capital spending for these options? In earlier papers from the ICB and the hospital board, the additional cost of maintaining the dedicated services on Crown Street was estimated at approximately £ 6 million per year. The cost of a rebuild was defined as “up to £336 m-£549m”. We pointed out that it would take up to 91 years for rebuilding to be cheaper than providing safe care at Crown Street.
Why is this paper not set in the context of the national Maternity crises, when hospitals with some of the configurations described here have had terrible outcomes for babies and mothers? Professor Marian Knight, Director of the National Perinatal Epidemiology Unit and MBRRACE-UK maternal reporting lead, said: ‘These data show that the UK maternal death rate has returned to levels that we have not seen for the past 20 years.” Clearly, the Maternity service has not benefited from moving Maternity into general and acute hospitals.
Why is there no mention of midwife staffing, nationally one of the major causes of stress, not specific to LWH on Crown St (see risk five below)? Liverpool Women’s can fill its permitted vacancies, but the staffing level for midwifery is inadequate.
Risks are asserted without proper evidence; the SLWH campaign produced a detailed response to these assertions (see here)
Why was the Save Liverpool Hospital Campaign excluded from this round of consultations, especially after previous assurances that we would be involved?
We demand:
Full public funding for LWH on its Crown St Site
Urgent investment in Maternity care to improve staffing, and facilities and tackle inequality to make Maternity safer.
Much improved staffing and funding for Gynaecology
A publicly owned, publicly provided NHS, fully restored, repaired, and rebuilt.“
The ICB claim;
“Risk 5 – Women receiving care from women’s hospital services, their families, and the staff delivering care, may be more at risk of psychological harm due to the current configuration of services” Stress levels are no different to the national average.
RCN press release April 2024 states that “24.5% of nursing staff are off work with stress, anxiety and depression. It is so widespread it accounts for 1 week of absence per year for every practising nurse.” Therefore, LWH is in line with the national average. NHS sickness data shows the average nurse took an entire week off sick last year due to stress-related illness
Please support our campaign. Sign our petition. Write to your MP and your councillors.
Donate to our campaign.
A more detailed analysis of the situation after this ICB meeting will follow as soon as we have had time to discuss it.
We need the ICB to come clean with the public and the Government and state clearly that the problems of the NHS are a result of chronic underfunding, creeping privatisation and outsourcing, which is sucking the lifeblood out of the NHS to no benefit to us, the patients, nor to the staff, nor to the economy, nor to our mothers and babies.


another thing to re-read and re-circulate is my short comment on the Case for Change.
https://labournet.net/other/2411/CfC.pdf
This is still relevant because in the Board Papers today, Fiona Lemmens makes repeated supportive reference to the Case for Change, e.g.
“There have been clinical senate reviews of the case for change and the counterfactual case; the case for change has been described as ‘compelling’ (North West and North East Clinical Senates).”
There is no acknowledgement of any criticism of the Case for Change.
Greg
LikeLike