Author: Mary

Introductory comments and information from Greg Dropkin
I’ll make some general points about the charges imposed on certain migrants for using the NHS. This stands at the border between two very big issues: immigration control and the hostile environment created deliberately by the government, and the attack on the underlying principles of the National Health Service. The idea of the NHS was to offer comprehensive healthcare for everyone in Britain, that is to say universal and comprehensive healthcare, publicly provided, publicly accountable, publicly funded through general taxation, and free at the point of use. Each principle is under assault, and the migrant charges are part of the attack.
Healthcare is no longer universal if certain people can no longer access it in reality, and it is no longer free if certain people are forced to pay for it. Listen carefully to what the last Health Secretary, Jeremy Hunt, had to say in 2017 in introducing the Govt response to the consultation on extending charges still further.
“Our NHS is the envy of the world and we have no problem with overseas visitors using it – as long as they make a fair contribution, just as the British taxpayer does.” And then, in the Overarching Principles, the gov’t stated “Whilst overseas visitors can access its services, in order for the NHS to be financially sustainable it is vital they make a fair contribution towards the cost of those services. It is therefore our intention to make sure that only people living here and contributing financially to this country will get access to free NHS care.”
That might sound reasonable, until you think about it. If only people living here and contributing financially to this country will get access to free NHS care, what about the 12 million people in Britain under 16 years old, none of whom are contributing financially? What about the chronically ill, or the Long Term Unemployed?
Of course, children will become part of the future workforce and if they manage to get a job, they will pay income tax. But so will migrants, who already pay taxes every time they go to a shop, who want to work and who are, on average, healthier than the rest of the population.
Why is the NHS in financial difficulties? Is it health tourism – i.e. people who come here just to use the NHS and then go home? No, that costs £70m per year, around 0.06% of the NHS budget. Could it be PFI, which costs £2bn per year? Staff shortages £3.7bn. Private contactors £8.7bn. Or government cuts to the NHS budget, £22bn per year? Blaming migrants diverts attention from the real causes of the funding crisis in the NHS. But there is more to the agenda.
In order to try to recover costs from certain people, hospitals and community services have to set up a complex system to check everyone’s entitlement to free NHS care, train staff to use it, allocate computers etc. In future that system can be aimed at anyone the government wishes to charge for any aspect of their health care. It is the thin end of the wedge to destroy the principle of free NHS care.
Then there is privatisation. Currently, care of the dying is exempt from charging migrants, but only if it is provided by a Community Interest Company or charity. In other words, this specific care need is being moved out of the NHS for certain people. In 2011, the govt floated the idea of requiring health insurance in order to get a visa. As we know, the long term aim of the various NHS reorganisations is to move to a health insurance system.
Attacking migrants access to the NHS puts clinical staff in a conflicting position. They are trained to deliver care on the basis of clinical need, not immigration status. Except for urgent and immediately necessary treatment, certain migrants must now pay upfront charges at 150% of the NHS tariff, before they are treated. Urgent treatment is billed afterwards. Migrants from outside Europe will be reported to the Home Office after two months if they owe the NHS over £500. When patient data is passed to the Home Office, it undermines the trust between patient and doctor.
People who are frightened of being charged or reported to the Home Office may delay or avoid seeking treatment. They are then at risk of getting more ill and ending up in A&E. Even with an infectious disease like TB, whose treatment is free for everyone, the stresses faced by migrants in the hostile environment including poor housing, mean they are at greater risk of developing the disease, and then at greater risk of delaying treatment, which is then a public health risk for the whole community. The NHS needs to trace people with infectious diseases to know who they’ve been in contact with, but fear of being charged or reported makes that even harder. In other words, in public health terms the policy is crazy.
There is an excellent overview in a recent article by Ed Jones, which I urge you to read along with a national leaflet from KONP, explaining the charges and busting the myths about migrants and the NHS. For example, about 20% of NHS workers were born outside the UK – so much for the myth that the NHS is a national, not an international service.
To sum it up, migrants are not causing the crisis in the NHS. The charging regime is inherently racist, no matter what Equality Impact Assessments the gov’t issues. We should oppose charging anyone in Britain for using the NHS, and we should defend all of its fundamental principles.
Rayah Feldman is here now. She is a social researcher in London who has studied both HIV and maternity, including several reports for Maternity Action, including the very recent “What Price Safe Motherhood?” She will explain in detail the real situation facing undocumented migrant women during and after pregnancy, as a result of the charges.

Talk at Liverpool.
This talk is based on a recent report for Maternity Action ‘What Price Safe Motherhood?: Charging for NHS Maternity Care in England and its Impact on Migrant Women’
Maternity care charging is a limited part of NHS charging but it’s significant because maternity care is usually regarded as special, so charging for it with no concession to its special status in relation to women’s and children’s rights makes the UK govt’s approach to it particularly problematic – and worth questioning.
NHS charging is a very significant part of bringing the border into everyday life. This is often called the ‘hostile environment’ – a shorthand for hostile environment for undocumented migrants, but actually creating a nightmare for all migrants as shown by the Windrush scandal.
Today I want to focus on what charging for mat care means in practice for the individuals it affects – and if time to explore a bit more its implications. In the workshops we can discuss ways of campaigning about charging and where mat. care might sit in such a campaign.
I will focus on 3 aspects of charging for maternity care in England as there are some differences in rest of UK
- Who is charged
- Charging procedures and practices
- Impact on women affected
- Who is charged
People with visitor visas, UDMs, expats. – people not ‘ordinarily resident’ in the UK. All other migrants who do not have ILR have to pay an Immigration Health Surcharge of £200 per year (doubling in December). This is paid in full in applying for a visa, so it’s £500 per person for 2½ years (£1000 in December) on top of visa charges of £1033.
Our study did not include expats but our advice service has had requests from women who were deemed not to be ordinarily resident because they worked abroad, or had been living abroad for some time. So we interviewed women on visitor visas and women who had overstayed earlier visas.
NB We interviewed 16 women – average length of residence – over 6 years before their last pregnancy.
- 2 women on visitor visas but both had British partners and were waiting to obtain spouse visas – so just in terms of the assumptions that a visitor is a tourist – this was not the case.
- 2 women were EU cits/ dependants – wrongly charged
- Some had come on student or visitor visas and become overstayers, and some were refused asylum seekers, some were very likely trafficked – one certainly was. Some who had overstayed their visas were trying to make further applications for leave, but this is difficult because not eligible for legal aid, and because of UD status had no money.
All those in this situation were very poor, and among the single women, often destitute as the following example shows.
Ayesha
Ayesha came to the UK for an arranged marriage. She had not met her future husband but he was ‘nice and caring’ when she spoke to him on the phone. They stayed together for about 4 months but she fled from him because he turned out to be violent and abusive. At that time she could not speak English and knew nothing about the UK. She survived by helping out different women she met in her mosque who offered her shelter in return for help with housework and childcare. When she became pregnant a family took her in for a longer period but made it clear she would not be able to continue to stay once she had her child. She was afraid to go back to her home country because she had run away from her husband, and she was also worried that her family would force her daughter to have FGM. She applied for asylum just before she was due to give birth.
She became pregnant while sofa surfing (often a euphemism for sex in exchange for accommodation). She did not stay with the father of her child. Ayesha’s story is a good example of how a woman’s immigration status can be dependent on their relationship. It also shows how irregular immigration status for women can give rise to a precarious personal situation in which women can be very vulnerable to abusive behavious by men.
In our study, only 5 of 16 participants continued to be in a relationship with the father of their last baby.
5 women were abandoned when they told their partner they were pregnant
3 – no information about partner (may have also been abandoned or may have been a brief relationship)
3 – separated from abusive partners during or after child was born.
Summary
- Women were charged who had lived here several years, sometimes had other children born here, or had British partners, or were incorrectly charged.
- Undocumented women without partners are particularly vulnerable to destitution and exploitation by men.
- Immigration statuses are fluid and changeable. Ayesha came as a visitor, became an overstayer, then claimed asylum
- b) Charging procedures
We did expect the women we interviewed to be very poor and living in difficult circumstances. But we also learnt from the study how harsh the charging regime is.
The charging rules
- Charges to migrants are levied at 150% of tariff charged to CCGs. So current maternity charges are £6993.63 for full package including antenatal care, delivery, and postnatal care. £1353 for termination. (Maternity care to CCG is £4662.42).
- Failure to repay £500 or more within 2 months results in being reported to the HO and can result in refusal of subsequent immigration applications or to re-enter the UK.
- Maternity care is considered Immediately Necessary – this means must not be delayed or refused if a woman cannot pay. But charges must now be levied in advance.
Charging practice
- Our study took place before statutory upfront charging was introduced so the timing of charging was arbitrary. 6 women were billed during pregnancy, 9 women post-natally or post miscarriage. 1 woman was not billed. Some were billed several months after giving birth. Some women were told the day their baby was born.
- Bills that women received were not itemised. Women who were charged in advance were not given advice on whether anything could be omitted. They were not told about possibility of payment plans, nor asked about their financial situation even though the Department of Health Guidance is very clear on the care that should be taken with vulnerable people (https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/742251/guidance-on-implementing-the-overseas-visitor-charging-regulations-may-2018.pdf See Chapter 7).
“When operating the charging rules it is very important to consider the position of vulnerable overseas visitors, including those unlawfully resident in our communities, both those who are exempt from charge and those who are chargeable.
“Overseas Visitor Managers (OVMs), and other NHS staff are strongly encouraged to speak to their safeguarding leads if, in the course of their work, they are concerned about the welfare of any patient. It can also be helpful for OVMs to build constructive relationships with local agencies which support people in various types of need, or to seek advice and information from relevant national agencies and organisations.” (DH Charging Guidance p53)
- Some women asked for information and were not given it.
- 2 women were wrongly charged and needed legal help to cancel charges.
- Some women were billed for previous births which took place years ago after they were billed for the most recent birth. This is now very common. Home Office officials are now often embedded with social services when they are asked for support by undocumented migrants. The Home Office then inform hospitals that someone had given birth there and was chargeable.
- Most women were not told anything about charging prior to receiving a letter or invoice.
- Subsequently they were harrassed with letters and phone calls, often from debt collection agencies. If English wasn’t their first language they could often not understand what people were saying on the phone.
The following are extracts from letters demanding payment which women had received:
Example 1
FINAL DEMAND FOR PAYMENT
Dear Sir/Madam
We wish to notify you that if this account is not settled within 7 days of this letter it will be referred to a debt collection agency and you may face litigation.
Furthermore, under immigration rules 320, 321, 321A and 322, a person with outstanding debts of over £1,000 for NHS treatment which are not paid within three months of invoicing, may be denied a further immigration application to enter / remain in the UK. If full settlement is not made, information relating to this debt will be provided to the UK Border Agency and may be used by them to apply the above immigration rules.
NB The demand about repayment of £1000 was out of date and inaccurate. The letter threatens litigation and provides no invitation to talk to hospital)
Example 2
One woman was told that as she had not paid
“the required deposit an invoice will be sent to the address you have given us. Please be aware that failure to pay this invoice may result in future appointments being cancelled.”
NB The letter made no reference to the fact that maternity care is designated as Immediately Necessary.
- c) Impact of charging on women
- Deterrence from attending care – women refused to attend further antenatal appointments. Natasha, on leaflet, would not go back for a checkup to find out why she had a miscarriage. One woman with high blood pressure went to hospital just before delivery after refusing to go to more antenatal appointments. One woman – the only one who paid in full, refused to go to NHS for anything. Even those who did go were scared.
“Whenever I’m going to the midwife I’m really scared to go. I’m not happy about going there now. I’m always scared. I don’t know what’s going to happen whenever I have an appointment with the midwife. I don’t know what I’m going to hear from them. Maybe they will stop me from getting care. In the hospital I was so scared.”
- Mental health– charging has a really bad effect on women’s mental health, increasing their stress and impacting on the family as a whole.
“When they were calling me and saying I have to pay, I have to do this, there was a point I felt like just dying. And my son was crying, I’m like, shut up! You know what I mean? I just screamed at him like, shut up! It’s just… It does have an impact (on the child) because I shouted at him when I wasn’t meant to. Because he was just a baby then, he was a crying baby. So the whole thing was just too much for me.”
- d) Conclusion
- This isn’t about recouping money for the NHS Of the 16 women interviewed, only 1 paid in full. 1 has 45 year repayment plan! 1 not charged because she claimed asylum. None of the others will be able to pay.
- It is well known and acknowledged by the government that mental health, poverty, homelessness, and being a migrant adversely affects pregnancy outcomes. So why are they not excluding maternity care from charging? In my view it’s racism in immigration policy combined with misogyny and hostility to family formation and reproduction among foreigners. e.g. Anwar Ditta case and the Primary Purpose rule in the 1980s and 90s.
- Also the approach to maternity deeply misogynistic. It sees women having babies in the UK only as maternity tourism, and refuses to see women as students, spouses, workers etc.
- The implementation of the charging policy is decentralised and not monitored and so is not consitent. There are no audits of the health impact of charging on women or its impact on deterring them from care.
- Failure to properly examine immigration status of chargeable people let alone their social and financial circumstances as advised by guidance gives rise to mistakes and undoubtedly to racial profiling e.g. in our study two Latin American women with EU rights were charged.
- Charging has an insidious impact on NHS. Divisions between entitled and unentitled become normalised, for example banners in hospitals saying “NHS Hospital Treatment is Not Free for Everyone” “The NHS is a Residency based provider and is not free for everyone.
Credit for images to Maternity Action and “noahs birth” by Kala Bernier is licensed underCC BY 2.0
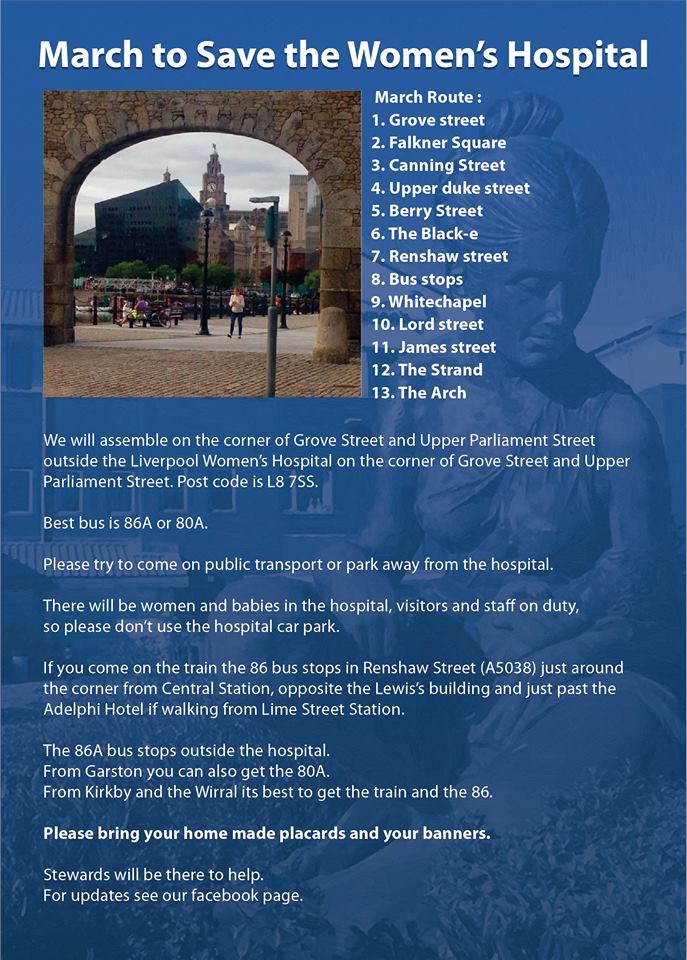
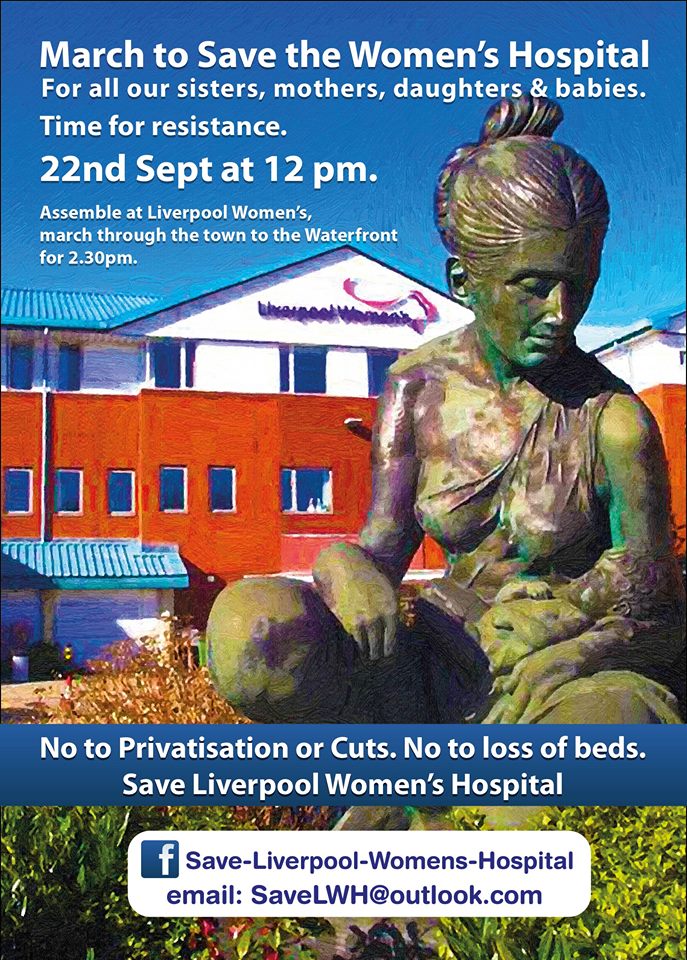
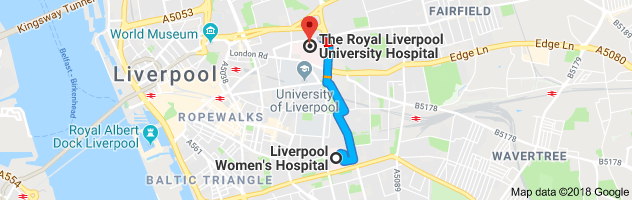
Last September, Emily Thornberry MP spoke at the end of our great demonstration to save Liverpool Women’s Hospital.
Emily is a senior Labour MP who speaks on foreign affairs for Labour in Parliament. She is the shadow foreign secretary. Last time we had our friend Diane Abbot M.P, speaking for the campaign so we have had good support from Labour’s women’s team.We were delighted to have her with us that day, and delighted to have Labour’s health spokesperson John Ashworth M.P. with us too.
It should now be clear that Labour is committed to saving this hospital. The battle though is not yet won. Plans to open consultation on the unacceptable plan to move to the Royal are still in place. PFI is probably dead, but the money makers and privatisers can still try to find another ripoff scheme.
The video has been made for us by Hazuan Hashim. It is lovely and important record of a great step in our ongoing campaign. We still haven’t won but we have made great strides and the hospital is still here.
Our fight and that of other hospitals, walk in centres and services goes on.The NHS has been stripped to the bone and only the good will and hard work of the staff keeps it going
The local and national campaigns for the NHS needs your help..

Integrated Care Partnerships are being developed across the country. There is a particular danger posed by chains of care homes owned by hedge funds and speculators gaining a say in our social services and our NHS. There are real risks involved with Integrated Care Partnerships. Only small section of health and social care professionals know about them but they will affect us all. This is not about day to day healh care or social care which clearly needs some level of integration.
“It’s integration of management systems, of financial purses, and
organisations, and it’s at the expense of the integration of true delivery of coordinated care that’s been going on and did not need Simon Stevens or Jeremy Hunt to tell us to do it.”
Do Labour Councillors and MPs and trade unions representing the workers, really want to go down that road? Can they please learn from the PFI scandal, step away from Integrated Care Partnerships? Can Trade Unions, Campaigners and elected representatives together put pressure on the government to fully fund NHS and fully fund social care and to drop the multi faceted privatising agenda?
Justin Madders MP, one of Labour’s Health team and a local MP, has published a criticism of Integrated Care Partnerships, especially their implementation without legislation going through Parliament or public consultation. The process of forming Integrated Care Partnerships fundamentally changes Social Services and the NHS. They gives the private sector still more access to the taxes we pay to fund our care. They reduce public and patient accountability and invite the hedge funds into the planning of our publicy funded health and social care. Profit is invited in to planning for our most vulnerable.
Hedge Funds are “an offshore investment fund, typically formed as a private limited partnership, that engages in speculation using credit or borrowed capital.” Hedge Funds are for speculation. Some of our readers will remember hedge funds speculation in Liverpool FC.
Now a chain of care homes is under crisis again and not a crisis through social care funding but from exposure to speculation. The Guardian reports
“US hedge fund puts Britain’s biggest care home operator up for sale
Four Seasons failed to pay off a portion of debt owed to H/2 Capital Partners”
The Care Home sector is attractive to capitalist speculators because it has an assured source of funding. The profit motive has not helped social care at all, despite the free market rhetoric. It’s not like a shop or other kinds of investment, this one has long-term government or local authority funding. Cash flow is secure. The funding that comes from patients and families is reasonably secure too because local authorities often help administer this. The cost to the older person and their families can be huge.
Families can be desperate not to have disruption. Changing a nursing home is a complicated task. On the basis of this very secure funding stream, it would appear, the speculators have borrowed on these businesses to invest elsewhere. In Integrated Care Partnerships NHS and Local Authority Social Care are being integrated with other providers, so the private sector are involved in the ICPs. The Kings Fund reported that “Integrated Care Partnerships can include hospitals, community services, mental health services and GPs, while Social care and independent and third sector providers may also be involved”.
There are four main players, in ICPs, the NHS, Local Authorities, voluntary sector organisations and the private sector. The sectors become more and more integrated. The private care home sector get a seat at the table, knees under the table, a strategic say in the funding and structures, and therefore a still more secure stream of funding for its speculators. Meanwhile our beloved elders are pawns in this game.
Public money and decision-making going into the private sector is not safe, a sector owned by hedge funds, who have no obligation to the public good. These homes can close when they want to. Regulation on peremptorily closing such homes is very weak. Local Authorities generally have to find new places for the residents. Many care homes have precarious financial situations Now the Guardian has posted the story of a hedge fund ordering the sale of the largest chain of elder care homes
The weight of the obligations to the elders in these homes must be on the owners and their backers. The full force of the law must be used to make them face their responsibilities but the laws are, as yet, weak. But once Integrated Care partnerships are in place it will be a shared risk. Investment is supposed to carry risk, tax funded services should not. The care home owners, US hedge funds, will be the partners in ICPs. We, the public, will share the hedge fund risks.
The NHS is free at the point of need and is supposed to provide all the treatments a patient needs There is more on this conflict here. The NHS is short of beds, the number has halved and this has contributed to the “winter” crisis. The Winter crisis is not caused by too many old people. After all, we have known about these people since their birth was registered, up to 112 years ago. We have known about increased life expectancy for years. Not planning for our elders is a sin of neglect on the part of governement. Its not surprise.
It is a joy and an honour as a society to have our elders live long and happy lives.
The winter crisis caused by shortage of beds and shortage of funds for social services. Social care is indeed in crisis. Unlike health care, Social Services provision is means tested until the person has lost nearly all their assets. Unlike the NHS there is no obligation to provide comprehensive services. Its a priced menu. You get what you can pay for. Private sector provision is planned for what makes a profit. The main function, such as elder care, can be subverted if there are better ways of making money. Southern Cross proved this but scandals have been swept under the carpet.
Many are familiar with the situation of older people needing medical care for age related illnesses, getting that from NHS but being charged for care for dementia because that does not count as medical need, but a social need.
This blurred boundary causes hardship It is reasonable to assume such blurring of boundaries will get worse under ICPs
There is a crisis in social care. It must be solved. But the money to solve that crisis must not come from hardpressed NHS budgets. It should come from general taxation, not NHS budgets.
Despite headlines that say Austerity is over, Local Authority social care budgets face the worst cuts yet .
“An analysis by the Local Government Association (LGA) reveals that, overall, councils will have suffered a 77 per cent decrease in the government funding between 2015/16 and next year, dropping from £9,927m in 2015-16 to £2,284m in 2019-20.”
Social care is short of money. Social Care Homes for the elderly were largely privatised many years ago. The iconic image of the time was of a little care home that a local GP might have set up, but this has long been bought up by the big chains. Some people will remember Southern Cross, where a whole chain went bust. Care homes can just close. Much of the private care sector funds come from Local Authority Social Services budgets, on a patient means tested basis. Other funds come directly from the old person and the family. The quality of care varies from brilliant to appalling
Care workers can be overworked under paid and over whelmed by the job. Full unionization and collective bargaining to represent the interests of staff are long over due. A well paid, well-respected staff, who are allowed some say in how the care is delivered make for good experiences for the elders in their care. When there are cut backs in funding the first people to suffer are the care workers
Much focus is on social care for the elderly but social care encompasses care services for children, and younger adults with physical disabilities or chronic illnesses. An activist and trade unionists conference on the whole issue of social care is planned in November
The system of care homes is not working in so many ways. Our campaign calls for a national care service fully funded from taxation but not to bail out the speculators
Care in the community for people with learning difficulties, and a variety of mental health issues have also been subjected to major funding shortages, and are largely outsourced, with all that means for staff wages, training, professional education and job security.
The staff of care homes, and in home care, are trained, managed and paid in a fundamentally different way from the NHS. Many of their staff have come from the NHS either by the original services being privatised or because they have chosen to move across. The staff development, which is the jewel in the NHS crown, is sadly lacking. Some staff perform duties, including giving out medication, well above their pay grade and their education/ professional qualification level.
It is the efforts and dedication of the staff which has kept the NHS and the care system afloat, though the boat is now leaking. The workers in the private homes are by and large doing their very best. Those with elected power have a responsibility to provide good care, quietly calmly and efficiently.
image Hedge Fund by Nick Youngson CC BY-SA 3.0 Alpha Stock Images

Please come to our demo, show your support for Saving Liverpool Women’s Hospital, on site,
Please support the call to fix the Royal Hospital!
Will you stand up to save the NHS?
What will you be able to say that you did about the attacks on our NHS? Will you get on your feet and show support for our NHS and our hospitals, our doctors nurses and midwives.
Our speakers are great but its the marchers who are the stars!
Come and hear our fantastic speakers
- Emily Thornberry MP,
- Dan Carden MP, who is committed to the reinstatement of our NHS, and is campaigning for the Royal Hospital to be fully funded and fully repaired
- Professor Wendy Savage, life long fighter for the rights of women and babies in healthcare and in giving birth,
- Doctor Alex Scott Samuel, from Socialist Health Association,
- Rebecca Smyth who lectures in midwifery
- Julie Ward MEP, who has helped the campaign for the successful Irish Repeal the 8th
- Jenny Hurley from Save Chorley Hospital,
- Sheila Coleman, Hillsborough Justice Campaigner
- Natalie Denny, local campaigner for sexual health for young people, and to making sure every woman can access sanitary products
 Wendy Savage has been given the prestigious award for ‘Outstanding Contribution to health and healthcare in the UK’ Wendy’s presence puts out campaign in a long line of struggles for women’s health and for maternity rights.
Wendy Savage has been given the prestigious award for ‘Outstanding Contribution to health and healthcare in the UK’ Wendy’s presence puts out campaign in a long line of struggles for women’s health and for maternity rights.
 Natalie Denny campaigns for young people’s sexual health, and for the homeless period
Natalie Denny campaigns for young people’s sexual health, and for the homeless period
Sheila Coleman is a fine example of a woman who never gives up, is never intimidated and fights for the rights of ordinary people, as does our campaign

 Rebecca Smythe has worked at Liverpool Women’s Hospital and now lectures in Midwifery. Rebecca is part of our campaign and can reflect the concerns of midwives in health reorganizations
Rebecca Smythe has worked at Liverpool Women’s Hospital and now lectures in Midwifery. Rebecca is part of our campaign and can reflect the concerns of midwives in health reorganizations


Why are we trying to Save Liverpool Women’s Hospital while the hospital puts out statements claiming all is well
As in Marvin Gayes’ version of “What’s going on”, it is very troubling. Our campaign to Save Liverpool Women’s Hospital has now been going since 2015 and has done much street campaigning. We have also done research and detailed studies of their plans. Not that it takes a genius to work it out.
 The plans which are presented as being all fine and dandy. The plans are part of what’s going on in the NHS, and some of which is downright dangerous. Sugar coated, press releases just don’t fool people anymore. We see the crisis. People are dying when they should not have died. The NHS is in crisis., and that crisis is manufactured by government policy.
The plans which are presented as being all fine and dandy. The plans are part of what’s going on in the NHS, and some of which is downright dangerous. Sugar coated, press releases just don’t fool people anymore. We see the crisis. People are dying when they should not have died. The NHS is in crisis., and that crisis is manufactured by government policy.
- The NHS does not have enough money because the government made the decision to underfunded it.If it were funded to match similar countries it would not have this problem. The money the NHS does have is frittered away to the private contractors who won 70 per cent of clinical commissions under the current flawed system. This cost the NHS, from which they made £831 million profit
- The NHS does not have sufficient beds because planners decided to close them as part of Government policy
- The NHS does not have enough staff because of government policies.
- Huge amounts of money have been wasted on PFI (PFI stands for Private Finance Initiative. It has been the dominant way of financing new hospitals since the late 1990s. As a result, the NHS spends £2 billion in PFI charges every year for its PFI hospitals in repayment and service charges. (That is £3,700 every minute).)
- Every PFI hospital has a huge mortgage round its neck to pay before it pays anything else. The Liverpool Women’s Hospital has no such mortgage.
- Money spent on NHS building projects gives millions to the builders and the financiers through PFI and the like. That huge investment has lacked scrutiny so major faults have been found in these big projects, not just at Liverpool’s flawed and unfinished Royal hospital. So PFI hospitals are scandalously expensive. Many PFIs are flawed and quite dangerous. “Site sources claim the cracks in the supporting beams stem from underlying issues with part of the building’s foundations
- The NHS lacks doctors and nurses because of government planning, by policy not by mistake. The Royal College of Physicians claims the government doesn’t even know how many doctors it needs Back in 2012 the government decided to train fewer doctors to prevent a “glut”.
- The LWH trust has a financial problem based on underfunding and a national problem with the maternity tariff. This will not change with the move. Indeed the PFI mortgage would exacerbate it
- The LWH shares many services with the Royal now. There are already problems with these shared services. The Royal cannot afford to subsidise the LWH.
- The team from LWH can and does operate at the Royal when there is a likelihood that long-term intensive care will be needed after the op. This quite common in the NHS.
- Nothing in these plans would stop babies being sent to Alderhey for operations.
The Government handed major control of the NHS from the secretary of state to the barons of the NHS, themselves ideologically and personally linked to major private health companies. Making money became a priority, moving the NHS into the “market” has caused further problems. Free trade agreements already threaten the NHS.
The decision to cut bursaries for nurses and midwives was damaging and difficult to explain if stability in the workforce was an aim. Many midwives will retire in next ten years as one in three midwives are in their fifties or sixties. This is one factor an even bigger gap, with more leaving than joining.
 The overwork, stress and under payment of staff makes spending £140 million on this seems even more unacceptable
The overwork, stress and under payment of staff makes spending £140 million on this seems even more unacceptable
There are two funding streams for the NHS, revenue which pays for salaries and day-to-day expenses, and capital which pays for buildings. Buildings surrendered because they are no longer needed are subject to the Naylor Review. The site would not be safe.Unless Naylor was revoked the site would be sold.
We believe the move to the Royal will enrich builders, enrich land speculators who would love the plot the Women’s now occupies, and do nothing to help the women and babies.
The Royal site is in the midst of a traffic hotspot and traffic pollution harms babies more than anyone, in the womb and when newly born. Travelling to and from such a highly polluted spot id not acceptable, even if filters were built into the air supply.
A landscaped green site is positively good for patients. Why should we lose that for our babies?
Maternity is an expensive sector for the NHS. “Admission to hospital to give birth is the single largest cause of admission to NHS hospitals in England”
Women’s health is a significant factor in the NHS with women on average experiencing 19 years of ill-health, and one-third having serious problems with reproductive health.
 We also value the calmness and kindness which is the ethos of the hospital .Giving birth in a calm quiet and caring place is great for the mother, the baby and the family. Patients who have been treated there for other conditions also speak highly of the ethos and care
We also value the calmness and kindness which is the ethos of the hospital .Giving birth in a calm quiet and caring place is great for the mother, the baby and the family. Patients who have been treated there for other conditions also speak highly of the ethos and care
The statement, and the plans published, make much of the safety gains of having the other hospital a bridge away. However in Birmingham women’s hospital which has such an arrangement, very ill women are still transferred by ambulance because that is safer than a trolley push.18 women were transferred last year out of the hospital and at least as many transferred into Liverpool Women’s Hospital. LWH is one mile from the new hospital. Broadgreen Hospial which is part of the Royal is much further away yet cooperation is not a problem there.
Recent CQC reports give the existing Women’s a good safety report. We reject the plans which reflect the maternity review, written by Conservative Peer Cumberledge, which is now increasingly discredited.
We need a hospital that focusses on women’s health, because we are not the same as men, much as we love some of them. We want to keep all the services together and not have them dispersed to the “community” where they are much more likely to be closed down quietly
In times of trouble we hold what we have, we do not let the good things go.
Save Liverpool Women’s Hospital
Fix the Royal
March for the NHS 22nd September 2018, 12 noon outside the hospital.
They say “Our preferred option for the future is to build a new Liverpool Women’s Hospital which will be physically joined to the new Royal Liverpool Hospital”.
We say no.

March for Liverpool Women’s hospital 2018 4
” We must save it”. Save Liverpool Women’s Hospital campaign has spoken with over 4,000 people this summer of campaigning.
 Some people have asked us questions about how and why the “relocation” of the hospital is being proposed. This then is an attempt to answer some of those questions.
Some people have asked us questions about how and why the “relocation” of the hospital is being proposed. This then is an attempt to answer some of those questions.
In a cash strapped NHS, should £140 million pounds be spent “relocating” a perfectly good hospital less than a mile down the road?
Should we be suspicious if this is in an area being gentrified?
Should a modern low-rise hospital in landscaped grounds, set back from the traffic, be rep
laced by a high-rise in the middle of some of the densest traffic in the city?
Should such a move be pushed on the false basis that the move would save money?
Should we take the risk of losing an exceptional hospital in a time and an environment so hostile to the NHS, in a situation of crisis, spring, summer, autumn and w
inter in the NHS? Or should we say, like the Merseyside Pensioners Association say “What we have we hold!”
 The Liverpool Women’s Hospital is explicitly safe. The CQC report indicates this and all sources confirm this. If you want more detail please see here
The Liverpool Women’s Hospital is explicitly safe. The CQC report indicates this and all sources confirm this. If you want more detail please see here
The day-to-day problems of funding for Liverpool Women’s Hospital come from the underfunding of the NHS nationally, and from an inadequate maternity tariff. The idea that savings from sharing some services at the Royal can bridge that gap or even pay for the £140 million move is not credible. Recruitment at Liverpool Women’s Hospital is traditionally good because it is a world-famous hospital.
The main decisions about the Liverpool Women’s Hospital are, officially, made by the Board of Directors of the Liverpool Women’s Hospital and the Liverpool Clinical Commissioning Group. Liverpool City Council Health and Wellbeing board has a say too. Liverpool City Council is working with other organisations as part of plans to integrate health and social care. This larger group could have a say too, though not immediately.
Just to be clear, it’s not the doctors, midwives and neo natal nurses making the decisions. Not here, not anywhere in the NHS. There are few doctors on the board. Clinical directors do not often attend the board meetings. Relationships between the hospital upper management and the staff are not always sweetness and light as the annual NHS survey indicates.
Liverpool Women’s Hospital has a regional role too. It provides services for women, babies and some men from across the region, into North Wales, and the Isle of Man. These services include the treatment of complex cases. Plans for the future of this hospital go to the other Merseyside Councils, in a joint committee for approval too.
 Liverpool Women’s hospital’s role as a neonatal centre has just been further developed by a grant of £15m funding to improve and upgrade its existing Neonatal Unit. Th re have been other improvements too in Outpatients department, and in the refurbished Gynaecology Unit.
Liverpool Women’s hospital’s role as a neonatal centre has just been further developed by a grant of £15m funding to improve and upgrade its existing Neonatal Unit. Th re have been other improvements too in Outpatients department, and in the refurbished Gynaecology Unit.
Merseyside and Cheshire have an Sustainability and Transformation Plan area that is supposed to plan NHS provision in its area (and make further huge cuts of almost £1billion across the area), and parallel to that is the Women and Children’s Vanguard , which nationally answers to the Maternity Review
The Maternity Review is pro privatisation, both in the use of for profit providers, encouraging dispersing services from hospitals and in developing costing mechanisms through the personalised budget system.The safety and effectiveness of the maternity review is called into question here .
Already many women have been charged for NHS maternity care based on their migration status even if they are living and working here, or if they are UK citizens returning here the costs are enormous.
T he pressure to use private providers, (one such organisation has been placed on enhanced surveillance) and to encourage home births are also part of the maternity review. Maternity care should respect the mother’s wishes AND must always be safe for mother and baby. Some of the ideas that over promoted natural child-birth by criticising provision that used interventions in childbirth, have already been rolled back since our campaign started in 2015. Home births for those who want them and for those for whom it is safe, are great, but the vast majority of women choose the safety of the hospital.
he pressure to use private providers, (one such organisation has been placed on enhanced surveillance) and to encourage home births are also part of the maternity review. Maternity care should respect the mother’s wishes AND must always be safe for mother and baby. Some of the ideas that over promoted natural child-birth by criticising provision that used interventions in childbirth, have already been rolled back since our campaign started in 2015. Home births for those who want them and for those for whom it is safe, are great, but the vast majority of women choose the safety of the hospital.
Many NHS budget crises, including that in Liverpool Women’s Hospital are temporarily supported by what’s called Transformation or Sustainability funds; it’s not quite the same thing as the STP areas, but came in at about the same time.
The NHS nationally must be formally consulted too about major expenditure. The NHS national structure is s complex. There is a set of slides available here but there have been changes since this was written. The laws changed in 2013 with the health and social care act and another major change is under way at present.
Consultations with the national NHS bodies are detailed and the ones about the Liverpool Women’s Hospital have been back and forth a few times, according to reports to the board.
 Two streams of money go into the NHS, Revenue for day-to-day spending and capital for major projects. Capital funding is the permission to spend money on long-term projects like new builds, refurbishment, major equipment and the like. NHS capital funding is not doing very well, falling for three years in a row ( Capital spending does well for the big corporations making a packet from it)
Two streams of money go into the NHS, Revenue for day-to-day spending and capital for major projects. Capital funding is the permission to spend money on long-term projects like new builds, refurbishment, major equipment and the like. NHS capital funding is not doing very well, falling for three years in a row ( Capital spending does well for the big corporations making a packet from it)
A bid for capital funding needs to be made if the current plans for a “relocation” are to go ahead. The plan is to relocate Liverpool Women’s Hospital to the traffic island that is the new Royal site (Prescot St, Liverpool L7 8XP)
There is a problem that this, and the last, government wanted to keep big capital expenditure off their books. They falsely believe that borrowing for investment can lead to a financial crisis. Its plain nonsense, details here. Keeping big borrowing off the government books has given big corporations like Carillon the chance to make a fortune from Private Finance Initiative which have resulted in hugely expensive and often badly built hospitals and schools.
At present there is no published source for the money for the Liverpool Women’s Hospital Boards plans. Unless there is a major turn in Government policy the money for this relocation will come via PFI, or possibly a loan from Liverpool City Council,. who will themselves have to borrow the money. Liverpool city council has its own major financial problem thanks to appalling austerity cuts from this government.
 The abominable chaos that is the new Royal Liverpool build has to be sorted out at huge cost. The full cost is not yet known, nor who will bear that cost. Never the less we are expected to believe that this will have no impact on decisions about money to relocate Liverpool Women’s hospital at the projected cost of over £140million on the same site.
The abominable chaos that is the new Royal Liverpool build has to be sorted out at huge cost. The full cost is not yet known, nor who will bear that cost. Never the less we are expected to believe that this will have no impact on decisions about money to relocate Liverpool Women’s hospital at the projected cost of over £140million on the same site.
Policy issues are decided by government and by their appointees in the NHS, like Simon Steven.They are not the polices the people of liverpool generally support.
There are two professional disciplines involved in planning health care, one is medicine which is the patient facing care and the other is health economics. The health economics planning in the last ten years have been disastrous, and politically committed to the privatisation and US model.
Lets look as some of the errors this group have made
1. Hospital beds numbers have been closed down but are desperately needed.
2. The internal market introduced to make hospitals compete has been an expensive disaster.
3. Staff shortages. Insufficient doctors , nurses and midwives have been trained. This is a planning failure, not an accident
4. Bursaries have been stopped.
7. Outsourcing and commissioning private companies to deliver health care has been costly and ineffective. Private companies made £831m profit from such contracts.
Doctors Nurses and Midwives and the related professions correctly want to be able to co-operate across hospitals, across disciplines. What stops this is not the physical placement of the buildings, but the trust system and the internal market.
Broadgreen Hospital and the Royal constitute one trust and are talking of merging also with Aintree . These buildings are much further apart than Liverpool Women’s Hospital and The Royal Liverpool University Hospital. Talk of an “isolated site” in this situation is a nonsense.
Long term intensive care at level 3 is not available at Liverpool Women’s Hospital. Short term intensive care is available at LWH. Those who need long-term intensive care are transferred to the Royal. 6 minutes away, by ambulance. This is less time than it would take to push a patient through areas of some hospitals. It would cost a lot less than £140m to upgrade the service at LWH. Services which do cause problems are ones that the hospitals already share.
 Our campaign is very realistic about the strengths and weaknesses of Liverpool Women’s Hospital. We heard some breath-taking stories whilst we were campaigning, some of wonder at lives started and others saved and some less happy. We met so many happy babies, and lovely children born there. Some of you we spoke to might like to share your stories on our Facebook page or in reply to this.
Our campaign is very realistic about the strengths and weaknesses of Liverpool Women’s Hospital. We heard some breath-taking stories whilst we were campaigning, some of wonder at lives started and others saved and some less happy. We met so many happy babies, and lovely children born there. Some of you we spoke to might like to share your stories on our Facebook page or in reply to this.
More than 40,00 people have voiced their opposition to these proposals. Our campaign wants
- to keep our hospital focussing on women’s health, the average British woman has 19 years of ill health.
- to keep maternity provision safe and away from traffic fumes and particulates
- to obtain better funding for the NHS and especially for maternity.
- to pay staff well, recruit, train and retain more staff.
- to oppose privatisation and PF.
- to end the rationing of care.
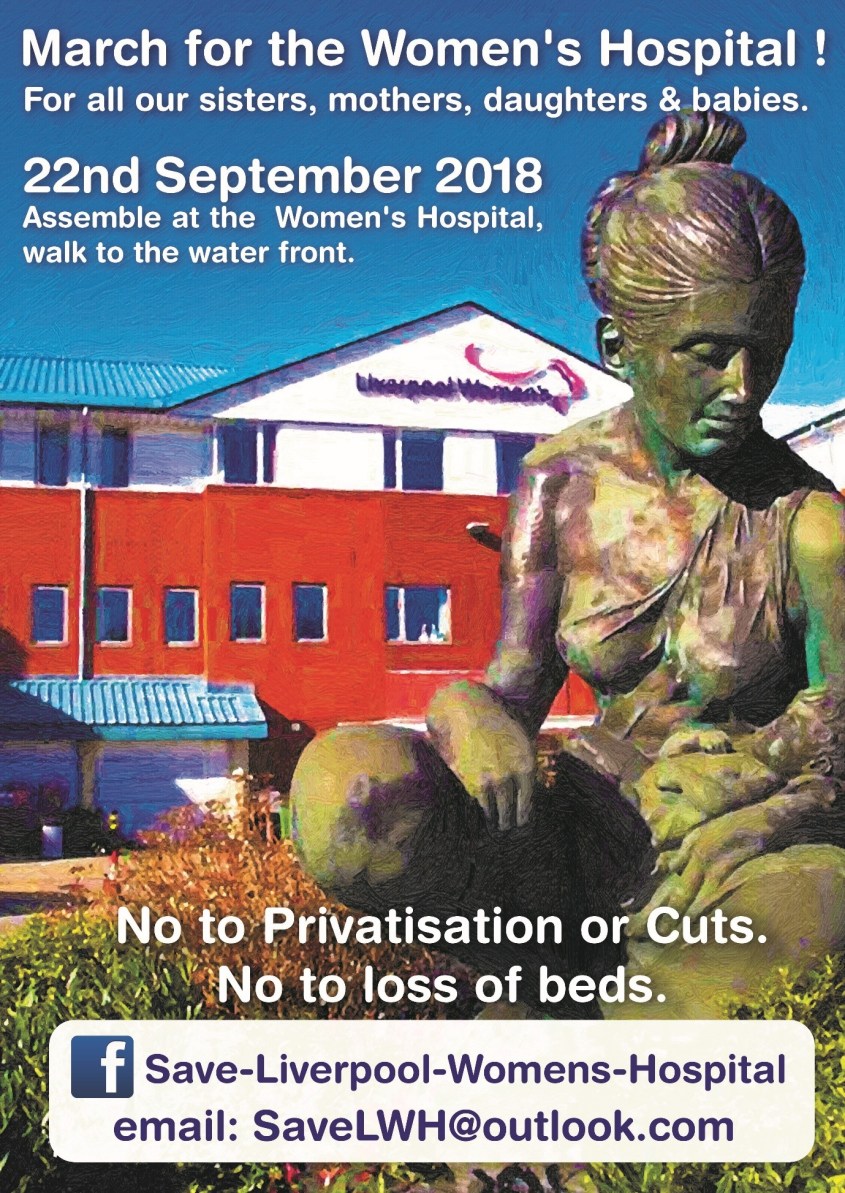 Please march with us on September 22nd 2018 at 12 noon to Save Liverpool Women’s Hospital and Save the NHS. This is the next stage in our campaign Fight like your grandmother did to get the NHS
Please march with us on September 22nd 2018 at 12 noon to Save Liverpool Women’s Hospital and Save the NHS. This is the next stage in our campaign Fight like your grandmother did to get the NHS
For all our sisters, mothers, daughters, friends and lovers.
Fund maternity services properly, nationally and locally
Protect and improve health care for women.
The NHS needs you. Bring the family. March for the National Health Service:
Fully funded. Publicly provided, not for profit. Free at the point of need and providing a comprehensive service. End the PFI scandal.
Repair and finish the new Royal Liverpool Hospital. Kick out the privatisers.
Pay the staff well. Bring back bursaries Tackle work-load
Please send solidarity greetings to use on the march and in the build up to the march
Follow us on face book Save Liverpool Women’s Hospital, emailsavelwh@outlook.com twitter @ lwhstays, blog Save Liverpool Women’s Hospital
March for the
Liverpool Women’s Hospital
22nd September
12 noon Liverpool L8 7SS, to Albert Dock, through town.

Our hearts and thoughts go out to the families of babies who died at the Countess of Chester Hospital Waiting, hoping and praying that a very sick new-born will come through leaves a permanent memory in the minds of the whole family. Thankfully many babies do make it through and grow into healthy children and adults.
Sadly some babies don’t make it and hearts break. How incredibly hard it must be for parents and families who also find that their baby’s death is possibly a murder. The emotional pain must be extreme.
Our thoughts go also to the staff who work in the hospital who have worked hard and professionally.
This has been a long chain of investigations some of which we have reported. We do not know and cannot comment on the guilt or otherwise of the case against the arrested nurse. That must go through the courts.
We do know that the NHS needs to reduce workload and increase the democracy in the management of staff, making more staff more confident to raise concerns.
The chain of events looks something like this. The numbers of deaths looked wrong. A report was commissioned. Then there was a follow up report, admissions of the most complex cases were restricted, the police were involved and now an arrest has been made. What happens now will be decided in the courts.
A year ago the Countess Of Chester Hospital published the following statement here




