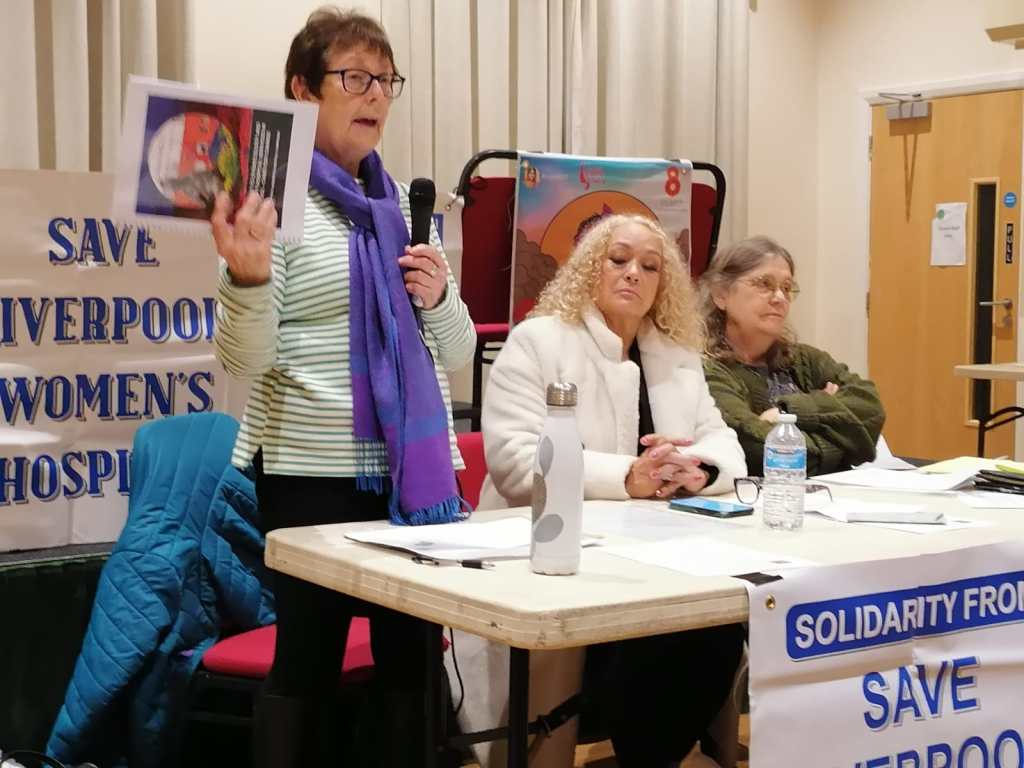
On Thursday, 24 July 2025, campaigners to Save Liverpool Women’s Hospital attended the meeting of the Cheshire and Merseyside ICB and asked a formal question, in writing, of the ICB about when the timeline for the future of the Women’s Hospital would be published:
“There is mention in the papers that a timeline for the next stage of the plans for Liverpool Women’s Hospital has been submitted to the chair of the ICB. When will the public be informed of this timeline?”
We were then promised that the timeline would be published on the website for Women’s Hospital Services in Liverpool.
We want Liverpool Women’s Hospital to remain at Crown Street, with improved funding, staffing, equipment, and cooperation with other hospitals, for the benefit of all our mothers, sisters, daughters, friends, and lovers, and every baby.
This is what the “Women’s Hospital Services in Liverpool” published. Their words are in italics. Our comments are in plain text and sometimes highlighted in yellow.
“The NHS is looking at hospital gynaecology and maternity services in Liverpool.
Most of these services happen at Liverpool Women’s Hospital, on Crown Street in Toxteth, which means they are separate from other hospital services, and this can sometimes create issues and delays with care.
The NHS is committed to finding a long-term solution that will improve the quality and safety of hospital gynaecology and maternity services, giving patients the best experience, wherever they are being treated.
Current timeline
What’s happened so far during 2025
March: Women’s Services Committee received a report into the autumn 2024 public engagement and approved the options process. The Board of NHS Cheshire and Merseyside also received the public engagement report, and it was published on the programme website.
(Our comment: Campaigners attended every meeting of this engagement, and not one of the meetings supported the position put by the ICB team. We produced a detailed rebuttal of their case, which we submitted to them. We are told they have considered the points we made, but no such consideration appears here. Their report continues…
What’s underway now and coming up (future dates still provisional and could change).
May to September 2025 – options process: Local doctors, nurses and midwives, those with lived experience of gynaecology and maternity services (members of our Lived Experience Panel), and other partners, have been coming together in workshops to develop potential options for how services could look in the future. Alongside this, work is taking place to understand what each potential option would mean for estates (buildings), finance and workforce (staffing).
None of the options discussed in the paragraph above are described or explained. These options are clearly getting out into the community, creating uncertainty and confusion. Why is that? Surely the ICB papers are the formal record of its business, and should include such vital details. The report continues…
July to October 2025: Development of a draft business case for the future of hospital gynaecology and maternity services in Liverpool, including potential options, begins.
October 2025: The Women’s Services Committee to review draft business case.
October to November 2025: Discussions with partners, including local NHS trust boards and local authorities, about the draft business case. At this point we will also start planning for an external review of the draft business case by clinicians from a different part of the country.
November 2025: Draft business case presented to private meeting of Board of NHS Cheshire and Merseyside.
By the end of 2025, we will be in a position to understand the next steps for the programme – it’s likely that we’ll be able to give an update about this in early 2026. It’s important to stress that no final decisions about what services might look like in the future will have been made at this point, and if the decision was to take forward a business case containing potential options, we would then continue with the NHS England assurance process, external clinical review, and planning the public and stakeholder involvement required.
Visit www.GynaeAndMaternityLiverpool.nhs.uk for the latest news on the programme.
End of report.
This long-winded and expensive project, which has cost many tens of thousands of pounds, continues while the hospital and the ICB are desperately short of funds. It leaves patients and the entire community in uncertainty. The real work of improving services at Crown Street is underway at the hospital. In another report to the same ICB meeting, the Women’s Hospital Services in Liverpool report confirmed that ;
Risk 6 – onsite quality and safety – the LWH team has made great progress over the last twelve months, and the score could be brought down, this will be discussed at Programme Board on 21 May 2025.
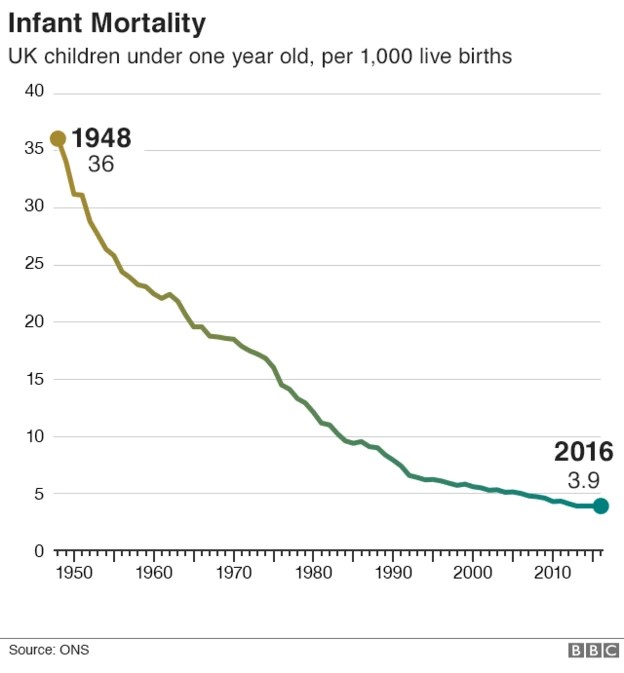
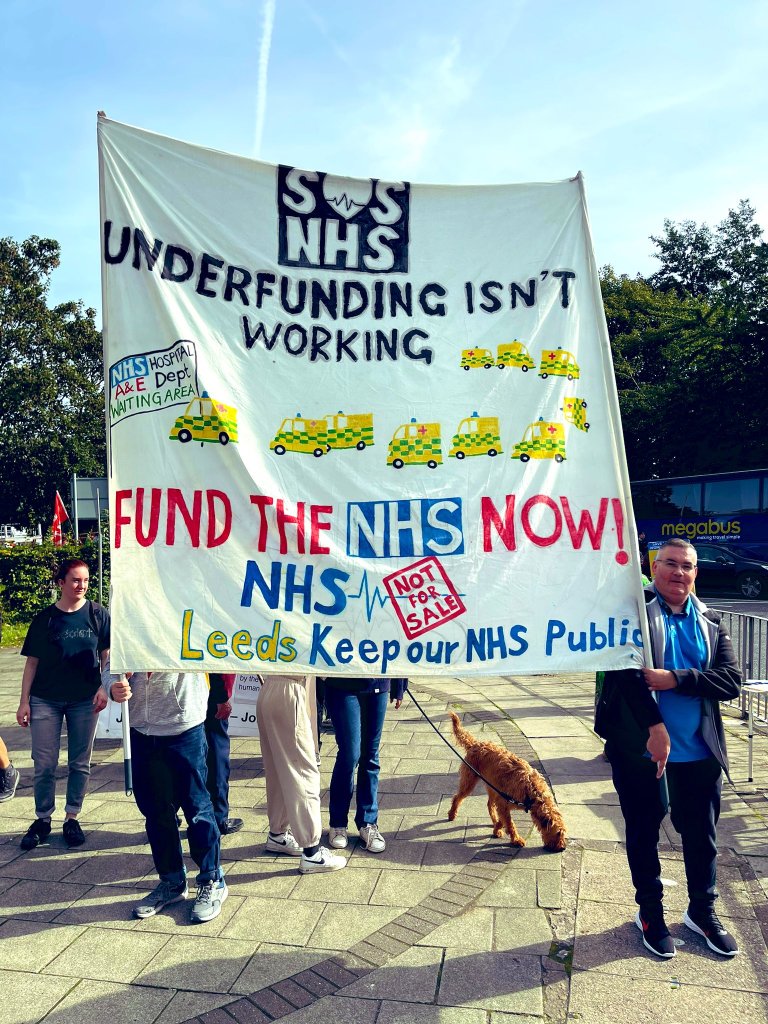
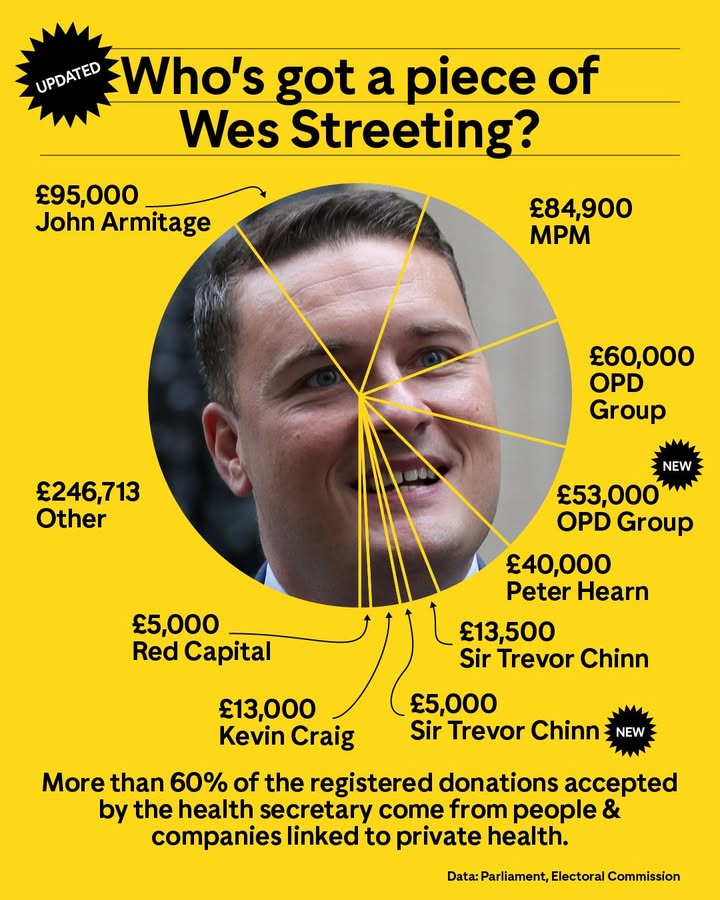
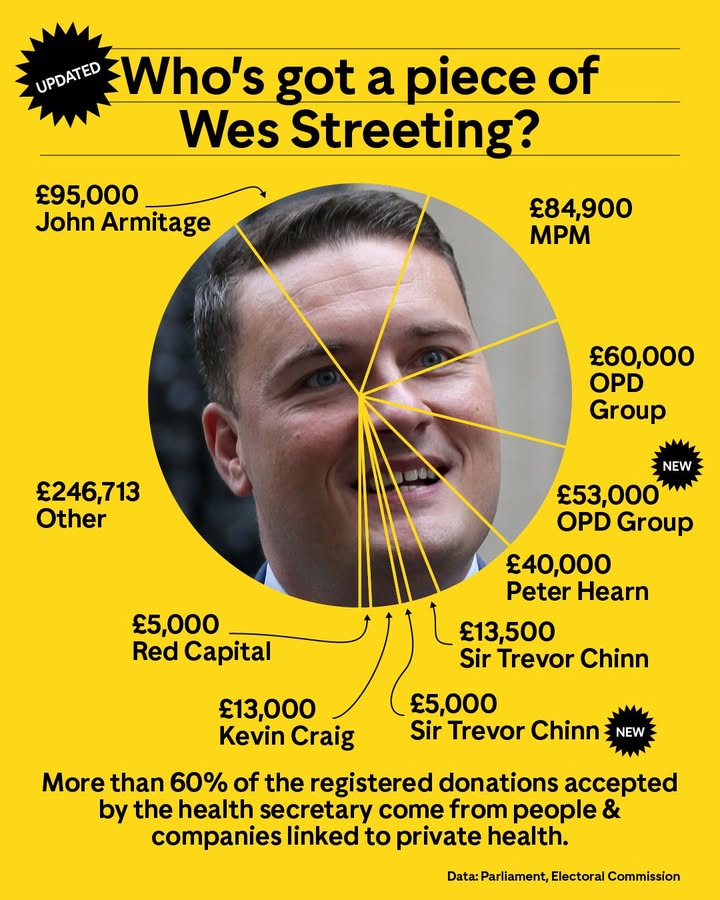
While the ICB’s process is happening, there is a Maternity crisis in England with report after report describing the grief and suffering involved. The NHS as a whole is underfunded, understaffed, and damaged by privatisation, and if this ICB meeting is anything to go by, it is getting even worse for patients and staff. We will report more of what happened at the ICB in a future post. Much of the rest of the ICB meeting was about further cuts and Cost Improvement Programmes.
The report of the Women’s Hospital services in Liverpool to the ICB in July confirmed that;
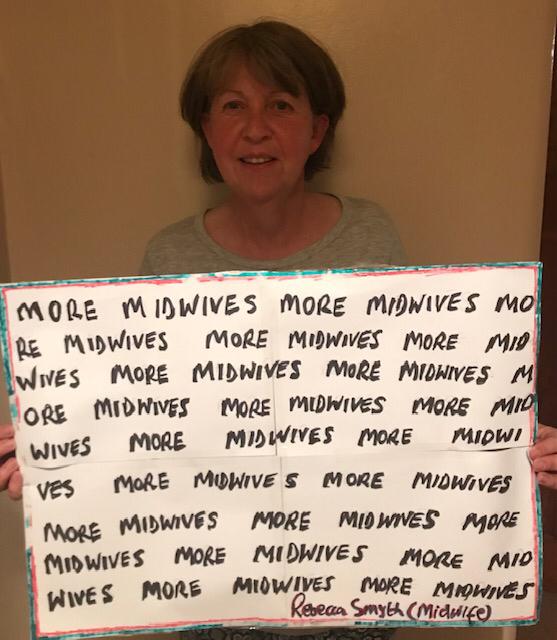
Risk 7 – a new risk has been added regarding staff reductions in the NHS and the potential impact on the programme. The programme budget has been agreed, however as the staff reductions are made throughout the year, there could be implications for the programme.
Liverpool Women’s Hospital is the largest Maternity hospital in the country. It is the Maternal Medicine Centre for the wider area, where other Maternity hospitals go for advice on complex cases. It should be well-funded, well-staffed, well-equipped, and well-supported. At the heart of the problems of Liverpool Women’s Hospital are;
1. The underfunding of Maternity across the country, an underfunding that has cost so many lives.
2. Utterly stupid policies, including the 2012 Act, meant hospitals were supposed to compete rather than cooperate with each other. This requirement has technically been removed, but the business model remains. Cooperation between the Women’s and other hospitals was difficult and expensive.
There should be NO staff reductions in this situation, especially as these reports from the same ICB (pages 146-150) from the Women’s Hospital Services in Liverpool Committee confirmed the real poverty many of us who use the hospital currently endure.
“Almost two-thirds of maternity bookers lived in the 20% most deprived areas in the country. Our partner hospitals in Liverpool University Hospitals Trust ranked in 2020 as having the most deprived catchment population of any acute trust (NICE and health inequalities, 2025).
“Based on recorded ethnicity and deprivation alone, 70% of maternity bookers 75% of emergency gynaecology admissions 50% of elective gynaecology admissions have at least 1 risk factor for healthcare inequalities…..64% of maternity bookers 71% of emergency gynaecology admissions 52% of elective gynaecology admissions live in the 20% most deprived areas in the country.”(Appendix to Women’s Hospital Services in Liverpool Committee report).
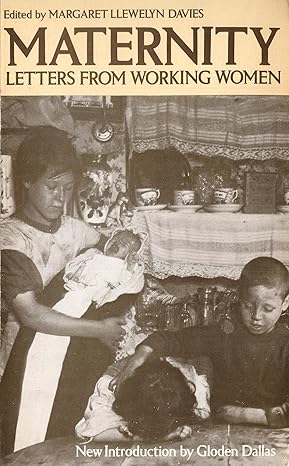
These papers also confirmed the significant gap between the lived experiences of decision-makers and the women using the hospital.
“There is a significant difference between demographics and experiences common among senior decision-makers and common among our patients. Designing services for the white and well-off would focus on about 10% of our maternity and emergency gynaecology patients.” (Appendix to Women’s Hospital Services in Liverpool Committee report).
The NHS has a duty of candour. Where is this duty here? The NHS belongs to the people. Why are such contentious discussions not described to the public, if the NHS belongs to us?
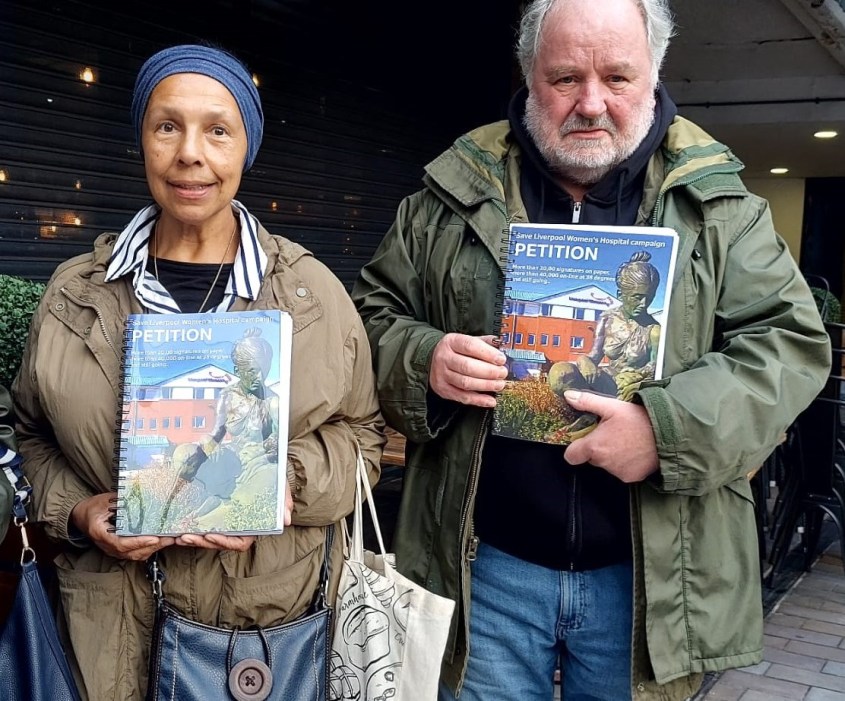
More than 81,000 people have signed our petition, to keep Liverpool Women’s Hospital at Crown Street, signed either on paper or online, and thousands have taken part in our protests. We have produced a detailed and comprehensive rebuttal of the ICB’s engagement process.

Keep our campaign growing to Save Liverpool Women’s Hospital. Sign our petition. Talk to your friends, family and workmates. Join our protest on September 28th.
This is part of the neglect of the NHS and of women’s health services. We demand that the NHS be Restored and Repaired!