Save Liverpool Women’s Hospital, the national maternity service, and women’s and babies’ healthcare. While we fight for Liverpool Women’s Hospital, we fight also for the whole NHS.
“As we go marching, marching
We battle too for men
For they are women’s children
And we mother them again.”
Together ordinary women and men can make a difference, and can put huge pressure on the government to improve our services and maintain that improvement. We cannot leave it to election promises, especially as neither main party at present is supporting the full restoration of the NHS.
The NHS is seen as the most important issue in the forthcoming General election.
Our campaign focuses on Liverpool Women’s Hospital. So, we asked local pregnant women for their thoughts.
“I think the most basic thing that women giving birth need is to feel safe, and to be able to have confidence and trust in the people who care for them before, during and after the birth of their baby. Continuity of care is so important, and while this is challenging to deliver, this should be the goal wherever possible. The Women’s has suffered some serious problems in the recent past, and work needs to be done to restore trust and confidence for the women and families who rely on this vital service. Women need to be able to access midwifery-led care, and be supported in their choices around birth and beyond. I want to feel secure that I will be offered treatments that will be beneficial (nothing unnecessary), that the midwives and doctors will listen to me and answer my questions, that they will seek my consent before they intervene, and that the quality of care and communication will be consistently of a high standard. I have experienced both excellent care and coercive and traumatic care at the Women’s in the past. I understand that there are serious system pressures that affect staff throughout the trust, but no woman should leave the postnatal ward feeling traumatised and vulnerable. Staff need all the support and training necessary to ensure this does not happen. Research demonstrates that birth trauma is a national problem, and I would like to see the Women’s taking a leading role in addressing this silent epidemic. As a tertiary centre and leader in obstetrics and foetal maternal medicine, the Women’s should be setting standards, not struggling to meet them.”
Another comment was:
“We need more focus on women with complex social needs as they have terrible experiences once they go in to deliver.”
We agree and say.
- Fight to save and improve Liverpool Women’s Hospital.
- Restore and Repair the whole NHS.
We need a national health service, funded at least as well as other European Countries, publicly provided, not for profit, available to all humans in the country, free at the point of need. This model is the safest and most economical model of healthcare. The US have a dog’s dinner of a healthcare model but it costs much more than the NHS and has many more preventable deaths.
The UK does not spend enough on our healthcare and wastes billions on private profits.
Governments know this and choose to involve big US corporations in the NHS so they can make a fortune, as our service runs on empty. The years of closures and mergers have done great harm and the last thing we need is more health care corporations to rip us off.
The U.S. has the lowest life expectancy at birth, the highest death rates for avoidable or treatable conditions, the highest maternal and infant mortality, and among the highest suicide rates. The U.S. has the highest rate of people with multiple chronic conditions and an obesity rate nearly twice the OECD average.
The years of closures and mergers have done great harm. In August 2023 a report said that “roughly 81 hospitals closed in the past 21 months, 6.6% of total hospitals.”
Liverpool Women’s Hospital requires about 25% more funding. This is because eighty per cent of its work is maternity, and maternity is badly funded nationally. However, funding for the whole ICB (NHS) in Merseyside and Cheshire is also a problem. One of the hospitals that cannot safely work within the given budget is Liverpool Women’s Hospital. The Board of Liverpool Women’s Hospital has set a budget for safety and must be supported in this.
The Cheshire and Merseyside Integrated Care Board provides the bulk of funds to the hospital with a small amount coming nationally from funding for specialist services. The ICB in turn gets its funding from NHS England. NHS England funds maternity through what they call the maternity tariff. This maternity tariff is inadequate for safe care. NHS England gets its funding from the Government. The buck stops with the Government.
The ICB said it has serious funding issues in its most recent report;
“Colleagues will be aware that the financial planning round for 2024-2025 has yet to be concluded. This is largely because provider financial plans [providers are the Hospitals and non-hospital trusts our comment] exceed the level of funding available and we remain in an iterative process [iterative means going back and forth] with NHS England as we seek to find the right balance between further cost improvements [cost improvements means cuts] and maintaining the core quality of services.
5.2 At the time of writing this report we were forecasting a deficit for the year in the order of c£150million (2.24% of turnover). We will be able to report back to Board verbally at its meeting in May [This meeting was cancelled].”
Sadly, Maternity does not feature in the priorities of the ICB despite reporting that many more women experienced a delay in induction of labour. This means that a woman has been told that her baby needs to be born soon and has come into hospital, to have the baby and then is kept waiting (and worrying) for more than 12 hours.
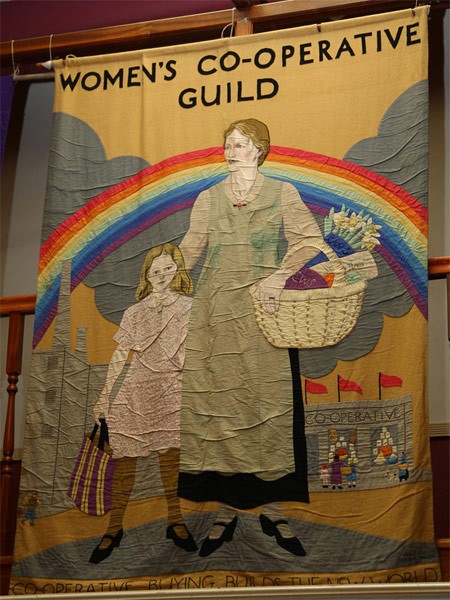
The NHS came from campaigns over many years from ordinary people, from trade unions in mining towns and working-class women’s organisations especially the Cooperative Women’s Guild who left behind a great record of their work in 1916 in the book ‘Maternity: Letters from Working Women, Collected by the Women’s Co-operative Guild’. Eventually, Nye Bevan founded the NHS as part of the 1945 Labour Government. It dramatically improved women’s survival giving birth, and the survival of babies.
Linked problems.
Women and children have been hardest hit by austerity and this has affected our health The prospects are grim indeed. In Liverpool “The life expectancy of women will fall by one year, and they will be in good health for 4.1 fewer years than they are currently. Although they are starting from a lower base, men will live 6 months longer than currently, and more of that time – 1.8 years – will be spent in good health.
Tell everyone who wants your vote to commit to real improvements in maternity services, a real commitment to the NHS. But do not leave it to MPs, get involved in the campaign to restore the full NHS and Maternity care. Suffragettes did not have a voice in parliament but they made themselves heard. We can campaign as well as our great-grandmothers.
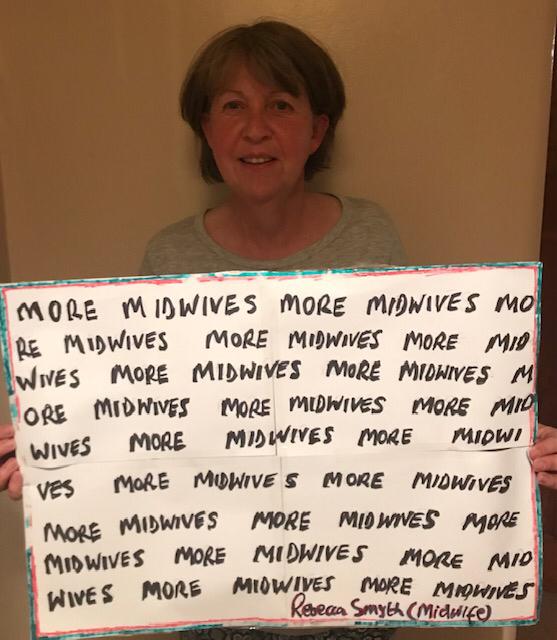
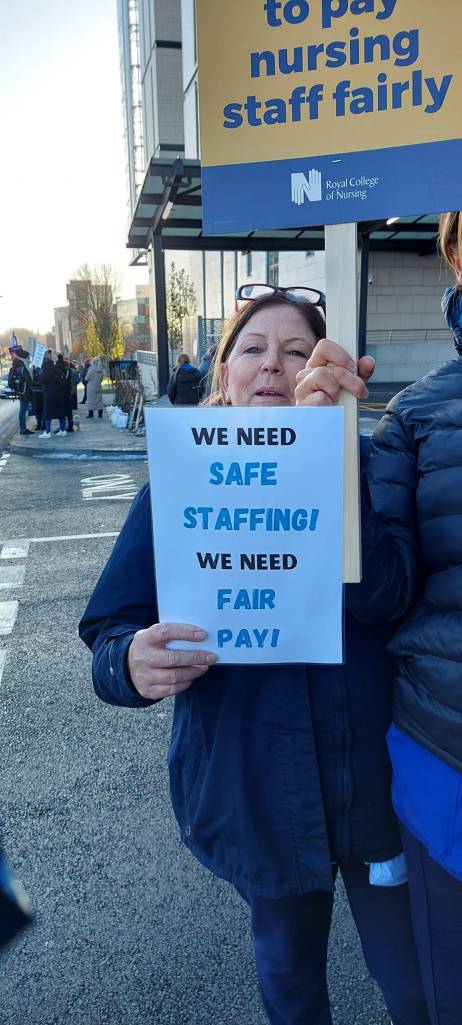
Save Liverpool Women’s Hospital. No mergers, no dispersal of services. We need more midwives. Fund all the maternity hospitals well. Staff them well. Staff should not be pulled from ward to ward just to manage day-to-day demands. Each ward should be well-staffed. Fund postnatal support. Fund safety-critical improvements. Fund and staff the specialist work of Liverpool Women’s Hospital. Make treatment timely and safe, without long waits for induction of labour. Make maternity services improve women’s mental health not damage it.
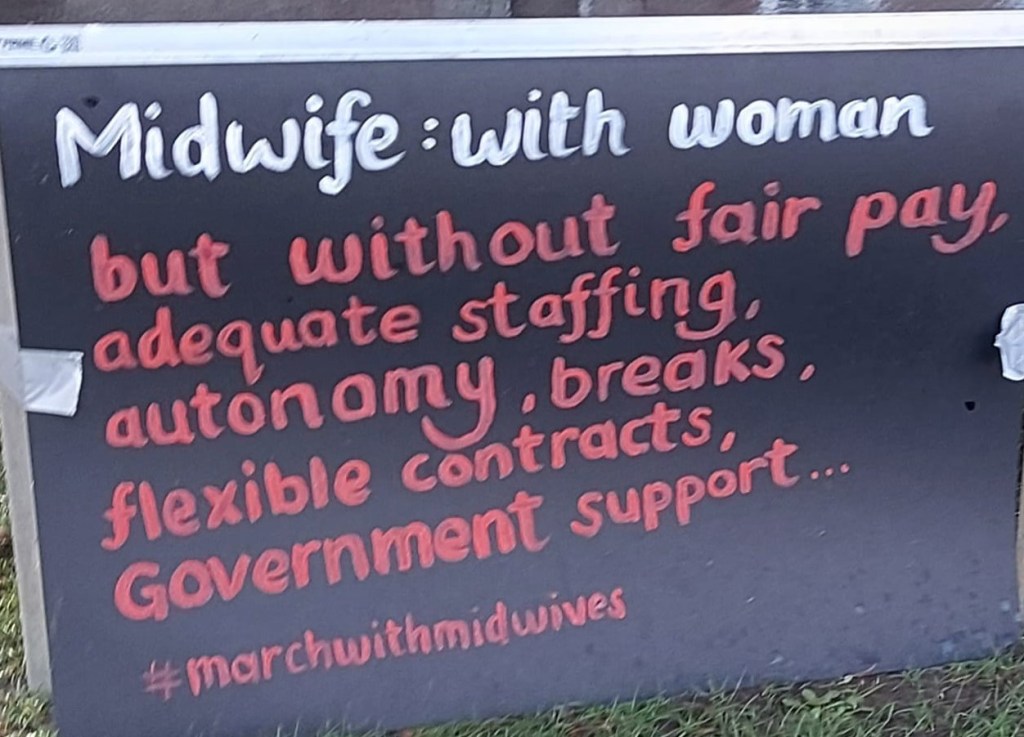
We need more midwives, and midwives need a professionally safe workload and good pay. It is hard to stay focused professionally if you are not sure where the next meal or heating bill is coming from or if you are working extra shifts to make ends meet.
Find out more about maternity here
Every life starts at birth.
As the suffragettes said
“Do not appeal, do not beg, do not grovel. Take courage, join hands, stand beside us, fight with us.”
It takes a weird level of cruelty to cut services for the birth of a baby but that is what has happened. Our campaign is far from alone in raising these issues. The government knows quite well what is happening in maternity. Multiple national reports have shown the crisis in maternity services for mothers and babies. These are some of the reports, all reported to Parliament.
2. Donna Ockendon,
3. Bill Kirkup
5. Maternity Services in England House of Commons Health and Social Care Committee
7. Report into the quality and safety of maternity services
The government responded with endless cuts to the NHS budgets. This year’s funding allocation for the NHS in real terms, taking into account inflation, is the worst in many years.
Improving maternity outcomes needs to be everyone’s business. Let us make it our business.
There are other NHS problems. Mental health care has been sliced, diced and privatised. Dentistry is simply unavailable to many people; GP services are in serious trouble through underfunding and crazy schemes to reduce our contact with a GP. Meanwhile, reports show that having contact with the same GP adds years to our lives
The service must respect and work with mothers. There should be continuity of care, not an impersonal production line.
Eradicate racism from the maternity service.

Fund the whole NHS.
No cuts or closures.
Raise the funding paid to all hospitals for maternity.
Raise the Birthrate plus staffing standards.
Protect and improve mother and baby health.
We support campaigns for the safety of mothers and babies in other ways.
- Outlaw sacking a woman for being pregnant and enforce that law.
- Improve maternity leave and maternity pay
- Improve paternity leave so fathers can play a role in those early weeks of life.
- End the two-child benefit cap.
You can take action now for the NHS as we enter the election campaign Send these questions to your candidates.

Join our campaign. Spread the word.