Update 08 01 2026
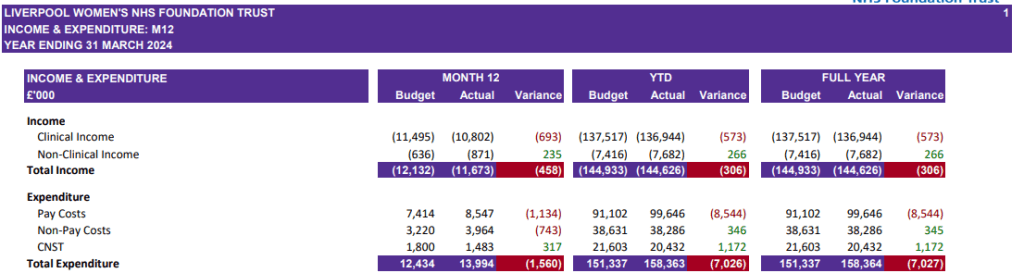
We are now expecting the report on the future of Liverpool Women’s Hospital to appear at the ICB meeting on 29th January 2026. However, other problems may intervene. The winter crisis, staff leaving at the ICB, and the likelihood of major redundancies at the ICB may get in the way. The ICB cannot and should not balance its books. It is in deep financial trouble due to cruel government cuts. The cuts the ICB is expected to make this financial year are brutal. We can see the damage to hospitals across the region. Liverpool Women’s Hospital cannot function long-term without a change in funding that allows for additional staffing and equipment. The two problems, funding for the ICB and funding for the Women’s Hospital, are interlinked.
Investment in healthcare grows the economy. It promotes health wealth and happiness. But that money must get to the staff, patients, buildings, and equipment, not to privatisers providing often substandard care.
Then we have the growing anger from bereaved parents, from women injured in childbirth, from overworked midwives and from the resident doctors. Patients are disgusted by year-long trolley and corridor care in Accident and Emergency, even before the winter crisis. We need more doctors,midwives, nurses and more hospital beds.
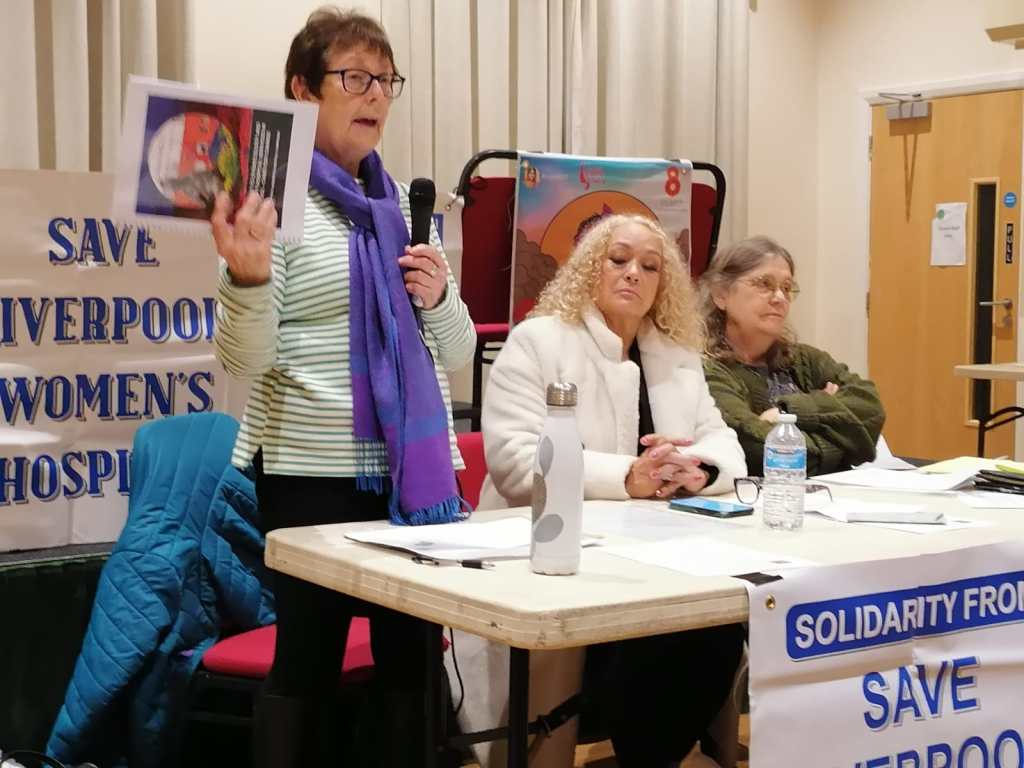
Campaigners will be attending the public section of the ICB meeting in January and will report back
What follows is an article from early December 2025.
What’s happening now, in December 2025, with the plans for Liverpool Women’s Hospital?
What is happening at Liverpool Women’s Hospital is part of a great set of problems in the NHS. Battered and damaged as the NHS is, it is still very necessary and much worth saving, for all our mothers, daughters, sisters, friends and lovers and every baby. “As we go marching, marching, we battle too for men, for they are women’s children, and we mother them again“
We stand with NHS workers and thank them for keeping the service going despite the appalling policies from this and recent governments.
Investing in healthcare gives great returns to any country in terms of health and wealth. We ask every reader to help us fight to repair, restore, and rebuild the NHS and Liverpool Women’s Hospital.
Grow our petition! It’s got 84,000+ signatures online and on paper. More will help – it gives the campaign a louder voice with the decision makers. No more Maternity cuts! We need more midwives! Fund Maternity and Gynaecology well across the nation.
For all our mothers, daughters, sisters, friends and lovers and every baby!
We campaign in Cheshire and Merseyside, and many other campaigns are working in different areas. The voices for the NHS and Maternity are growing louder and louder. Please amplify these voices.
Latest news
The ICB (Integrated Care Board ) is the governing body of the NHS in each area. Ours is the Cheshire and Merseyside ICB.
At the ICB meeting on November 27th, 2025, which campaigners attended (as members of the public), we were told that the item was not to be discussed, neither publicly nor privately. We had sent written questions. They replied:
“Unfortunately, due to a number of other urgent items which require immediate discussion, the Women’s Hospital Services in Liverpool item will now not be
included on the agenda for this month’s private Board meeting, and will instead be rescheduled.“
“When it takes place, the private Board discussion will be focussed on how we move forward with the programme, taking into account the extensive options
work that took place over the summer, and will not involve making final decisions about how services might look in the future.”
We had asked in a written question whether the ICB would be discussing the costs for relocation versus staying at Crown Street, as seen in the hospital papers. The additional cost of keeping the dedicated services on Crown Street was described as approximately £6million extra per year. The cost of a rebuild was defined as“up to £336 m- £ 549m“. We pointed out that it would take up to 91 years for rebuilding to be cheaper than providing safe care at Crown Street.
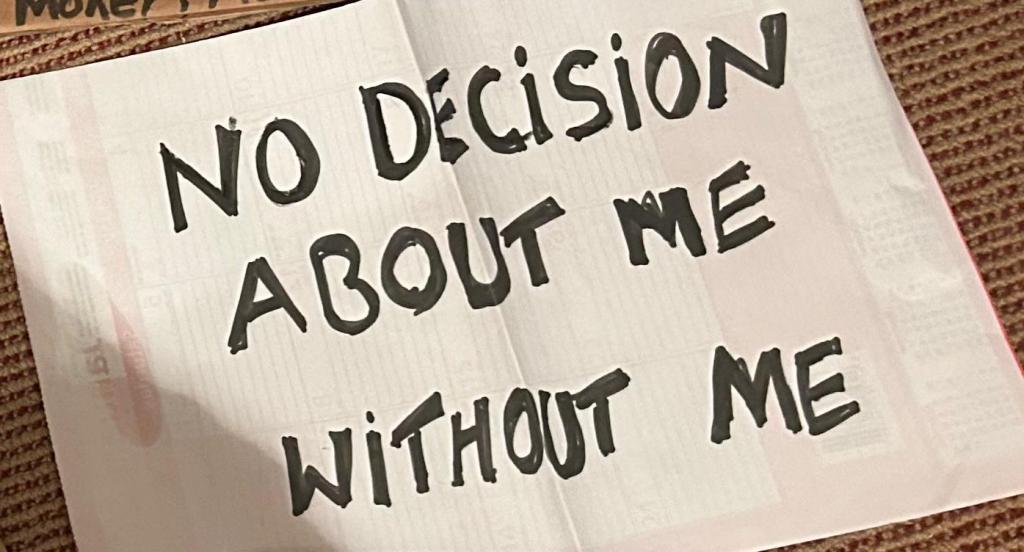
This campaign would like to know what was involved in “the extensive options work that took place over the summer.” We would like to know who was involved in these options and where they were reported, because we cannot find them reported in either the ICB or the hospital board meetings. Why the need for secrecy? Why not involve concerned members of the public? We wrote and asked to be involved in these discussions and were refused. The NHS is not a private corporation; much as some rich companies would like to acquire it, it is still a public body founded by the people, paid for by the people and staffed by the people.
The ICB also said they would still discuss it in private when the item returned to the agenda. We were told there would be some news in the new year. We have also been promised meetings with the ICB chair and the Hospital Group CEO, so we might find out more.
The future of Liverpool Women’s Hospital remains uncertain. What is certain is that Maternity, nationally and locally, must be better funded. It is summed up in a simple fact that we need more midwives.
There is a reluctance in the NHS to say that underfunding and understaffing, too few midwives, and too few hospital beds are core problems. Well, we will say it for them.

Since the 2016 discussion about the future of Liverpool Women’s Hospital, there have been suggestions that it would be rebuilt near the new Royal. Many people still believe this. We neither believe that it will be rebuilt nor support rebuilding it. The Crown Street site is a good building. The staff are a good team with a global reputation. The women and babies of Liverpool need and love that hospital.
Many other Maternity services nationally operate in appalling buildings. The Health Service Journal reported that” Many Maternity and newborn units are at ‘serious risk of imminent breakdown’, regularly hit by leaks and floods, and too cramped to provide the necessary care, an official NHS England report admits. There was a detailed report published by the NHS about this last year. The poor buildings should be rebuilt, not Liverpool Women’s Hospital. Many other hospitals urgently need a rebuild, but the plans for that are delayed.
Improvements at Liverpool Women’s Hospital
There were reports last year that a deteriorating patient’s team was being developed at Liverpool Women’s Hospital, and we hope that this is now in place. This is much needed. Other improvements are in place, including bringing the “soft facilities management services” (cleaners, porters, etc.) back in-house. The Case for Change states that “As part of elective recovery funding, £5m has been provided to establish the Liverpool Women’s Hospital site as a centre for gynaecology procedures. This includes four state-of-the-art procedure rooms developed to free up capacity in theatres and create additional clinic space for more minor operations, and will enable up to 4,200 additional gynaecology procedures every year. In addition, Crown Street now hosts a community diagnostics centre with CT (computed tomography) and MRI (magnetic resonance imaging) from 8am to 8pm, and urgent access to CT 24/7, which has delivered improved access to scans and reduced transfers for these diagnostic tests.

The CQC report in August 2025 stated that Liverpool Women’s Hospital has improved.
“Karen Knapton, CQC deputy director of operations in the north west, said: “We were pleased to see that leaders and staff working in Maternity services at Liverpool Women’s Hospital had acted on our feedback from the previous inspection and worked hard to make improvements. Women and people using this service now had a much safer and improved experience of their care and treatment. Behind this was an improvement in how well-led the service was, which in turn supported staff to provide better care.
“For example, it was positive to hear that leaders had improved staffing levels. Women using the service told us there were enough staff to meet their needs, and they were treated with compassion and kindness. It was great to see this reflected in a recent people experience survey, which found 94% of women felt they were treated with respect and dignity.
“Overall, the Maternity team at Liverpool Women’s Hospital should be proud of the improvements our inspection found. They should use them as a foundation to keep building on.”
We applaud these improvements. Nowhere does the CQC mention relocation, nor have earlier, less complimentary CQC reports mentioned this.
Underfunding and understaffing have caused severe damage to mothers, babies and staff. More has been paid in damages from the service than has been spent on the whole national Maternity service.
Scandalously, “the potential cost of Maternity negligence claims in England since 2019 has reached £27.4 billion, which significantly exceeds the estimated £18 billion budget allocated to Maternity care over the same period“. We say improve the services and reduce the damage! When will the government focus on the needs of mothers and babies?? The voices of women and their families must be even louder on these issues.
Co-location has not been a success for maternity. It is not the only problem, far from it. Cuts and underfunding have been a disaster.
The “Case for Change” also says, “All other specialist centres for gynaecology and Maternity services in England have co-located acute and emergency hospital services.” We say that this co-location of Maternity in general hospitals has not proved to be a cure-all for Maternity crises, far from it. Maternity, despite being based in acute and general hospitals, is in crisis.
Although a standalone site, Liverpool is not one of the 14 Maternity providers involved in the so-called “rapid” national investigation of Maternity and newborn baby care across England. The Labour Government promised a rapid enquiry, but this enquiry is now not reporting before Christmas and might report sometime in the new year, and will not hear from bereaved parents.
Fourteen general hospitals ARE included in the national Maternity crisis, and others have been the site of some of the Maternity scandals. The Shropshire Okendon enquiry indicated that the management did not give Maternity due attention, nor did the Morecombe Bay hospital management give Maternity due attention, even after the big report.
It’s not just Maternity that is suffering in the NHS.
The women’s hospital reflects the many problems besetting our healthcare system. Books have been, and will be, written about this. We are trying to change the situation. These are the core issues.
- For many years now, the NHS has been underfunded and understaffed compared to other countries, and this has been a clear government policy.
- The organisation of the NHS has been damaged by pro-market legislation, especially the 2012 and 2022 Acts, which set hospitals up to compete against each other and allow for-profit interests to have a much greater say. Lord Darzi, in his report for the incoming Labour Government, described the 2012 Act as a“calamity without international precedent” that “proved disastrous”. For Liverpool Women’s Hospital, it meant that cooperation between hospitals proved very difficult, and the high cost of the foundation trust system was too much to bear. Not keeping to an impossible budget made them constantly under pressure.
- Maternity and gynaecology, across the country, suffered badly, with one in six Maternity units closing, and standards deteriorating. A major Maternity crisis developed with standards and staffing suffering, resulting in damage to mothers and babies.
What were the greater issues that pushed the Liverpool Women’s Hospital to the back of the agenda? They were hugely based on funding, cuts and the winter crisis. We will write about them in another article soon.
“You get one chance to deliver a baby safely. There are no reruns or repeats. The accoucher must get it right every time. To do so, the midwife must be supported by her colleagues, midwifery management and work within a fully safe environment. Alas, with the fragmentation of our NHS, top-down draconian management, our mothers, their babies and our midwives are given short shift, and they become the victims of often tragic circumstances. There is a woeful shortage of skilled midwives. Anyone can deliver a baby, but it takes a skilled midwife to do so day in day out safely and with professional accountability,” from our campaigner Stephanie (below)