Black Maternal Health and Anti-racism Action in the NHS: Issues for Liverpool and beyond.
We honour the women in Liverpool who have suffered or died because their treatment was affected by conscious or unconscious racism. The best way to honour these sisters is to campaign ever more strongly against both inadequate Maternity care, nationally and locally, and against the insidious rise in racism in this country. Anti-racism education in the NHS can save lives.
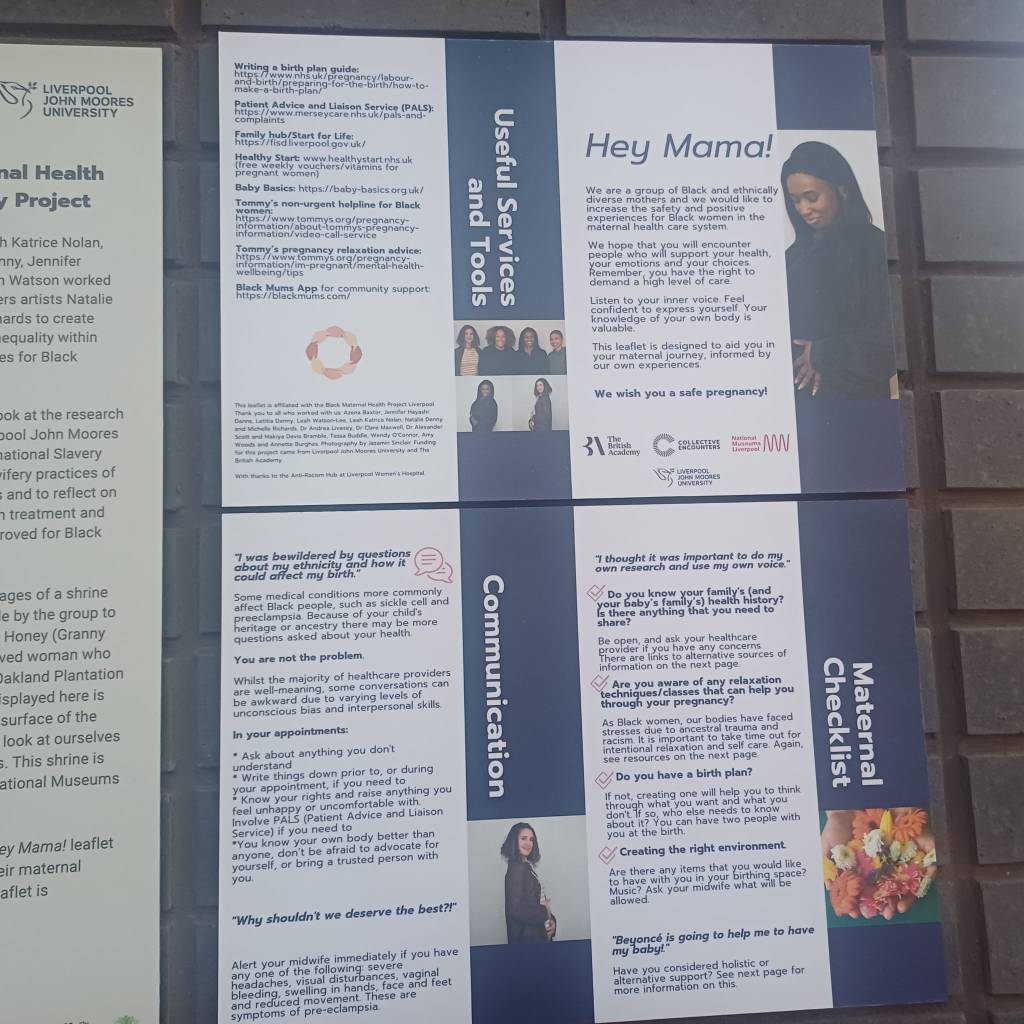
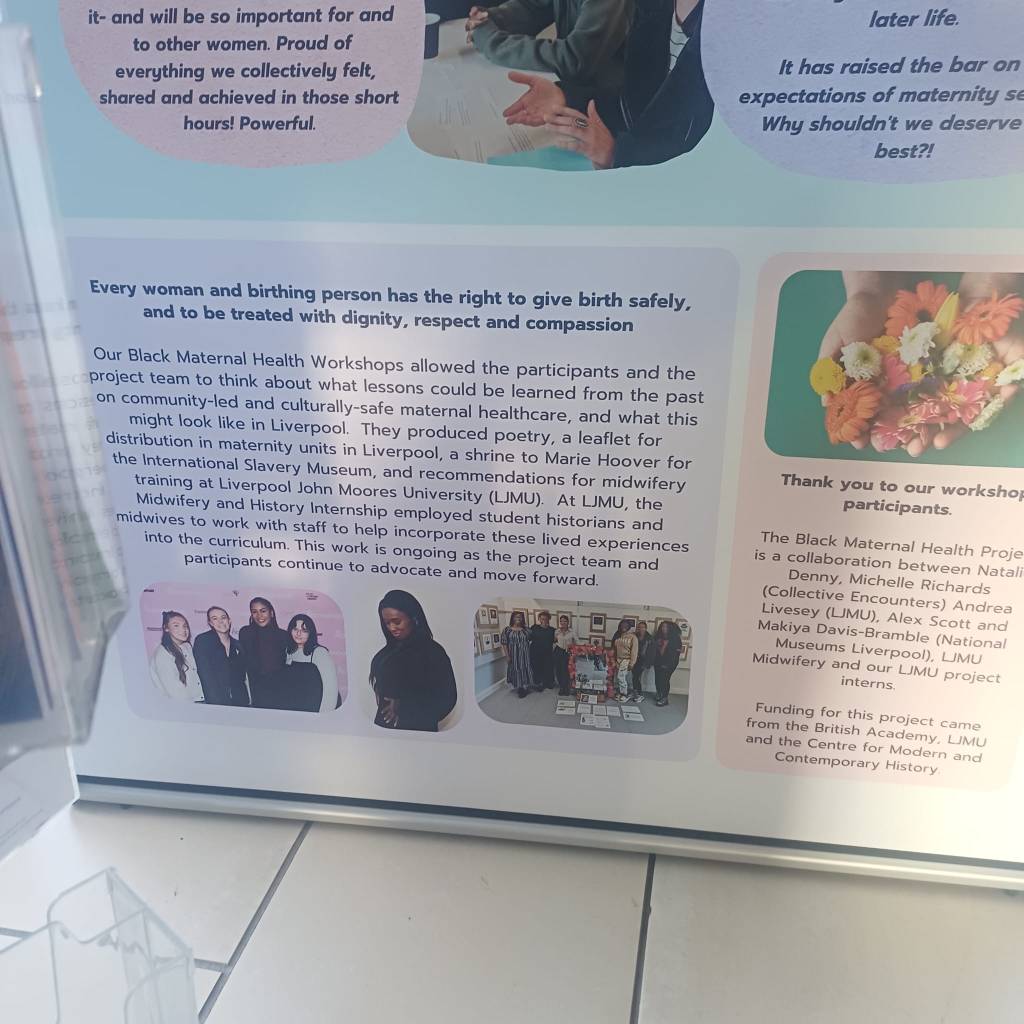
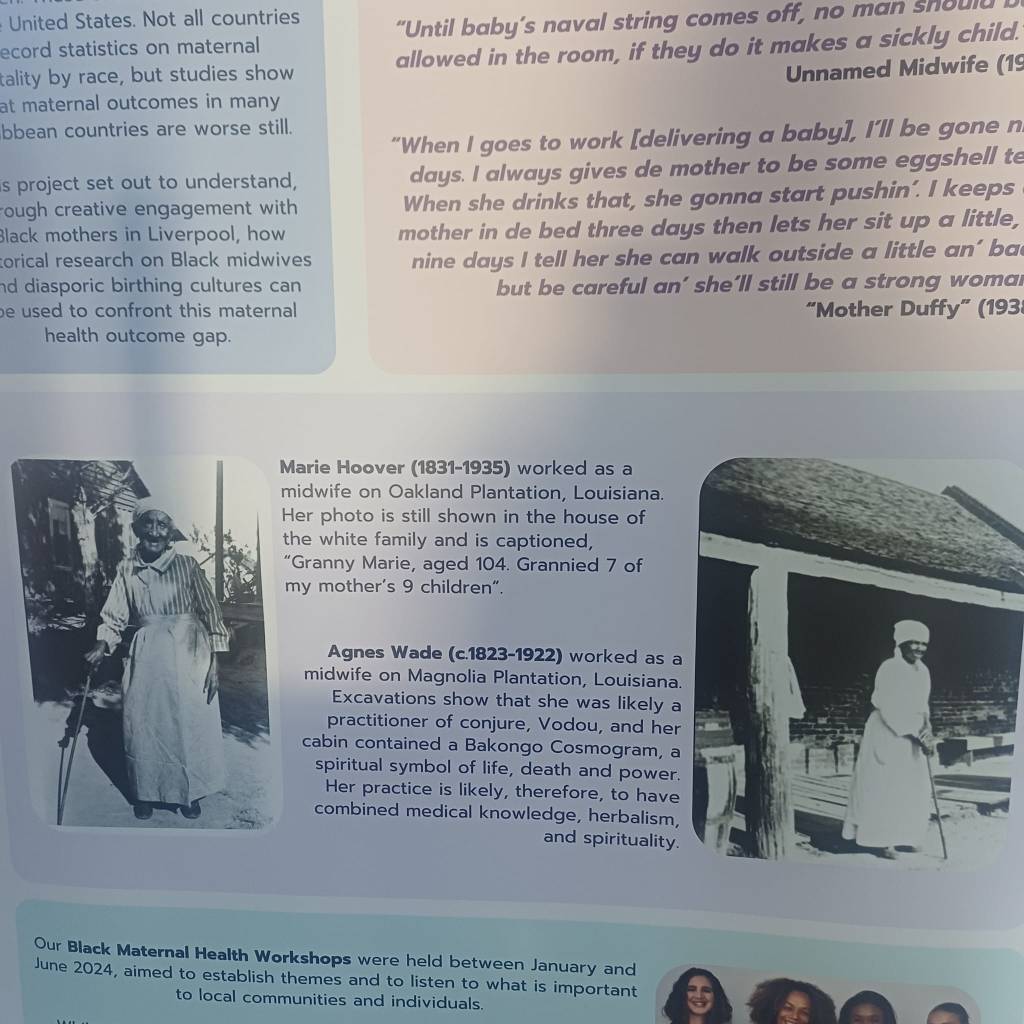
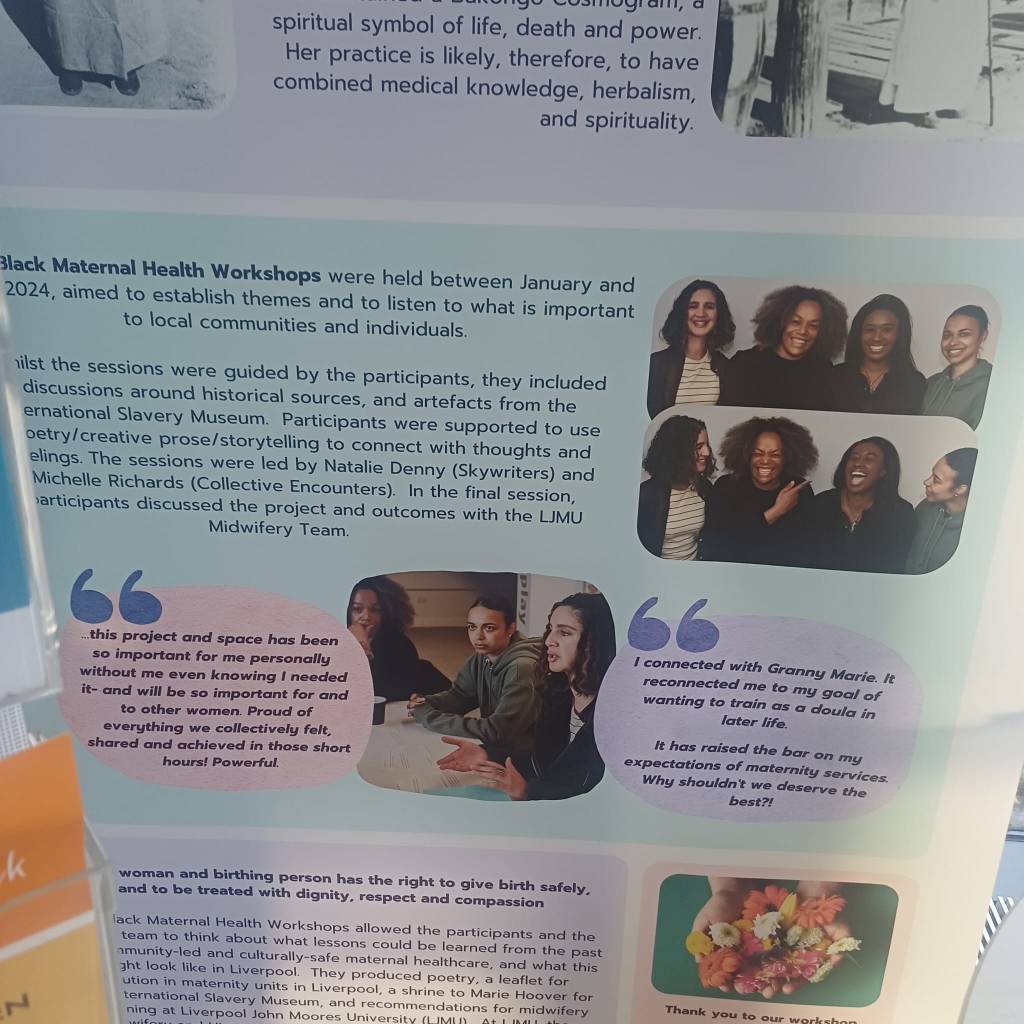
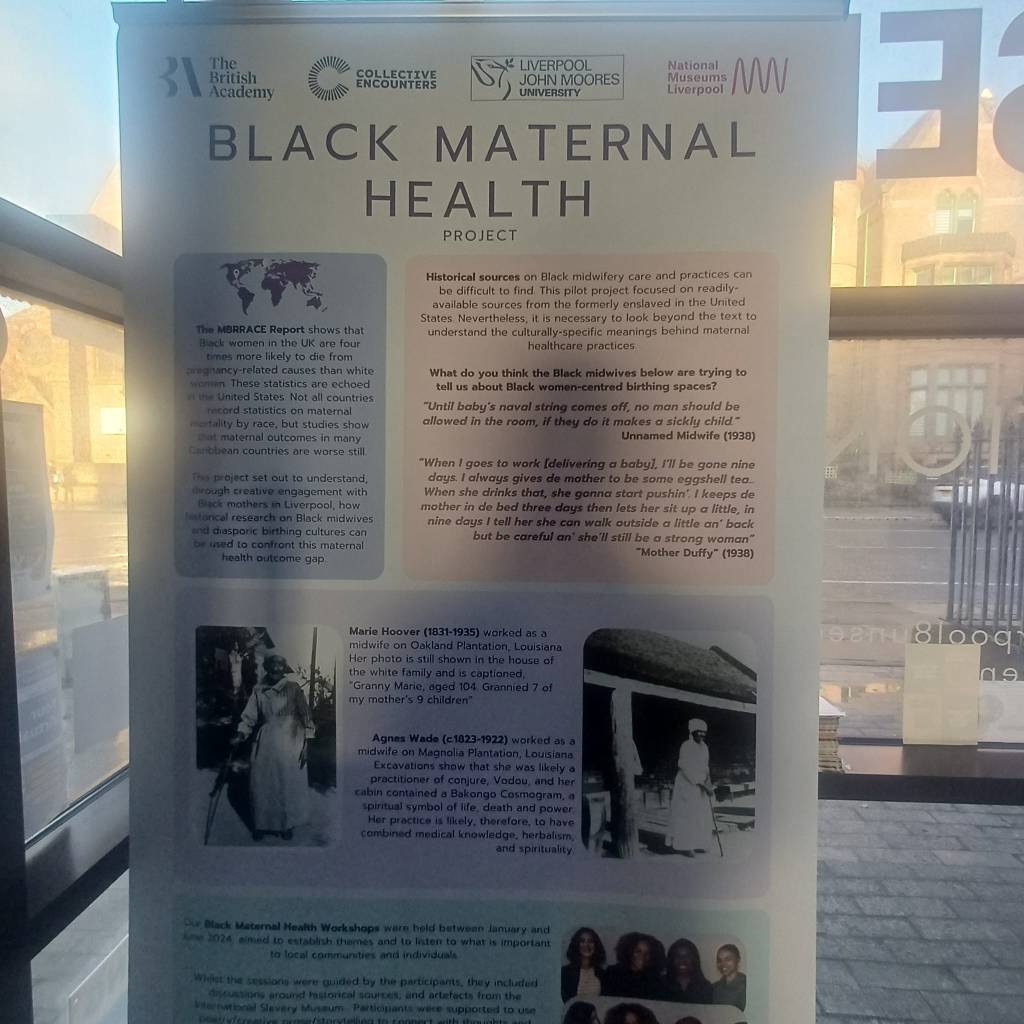
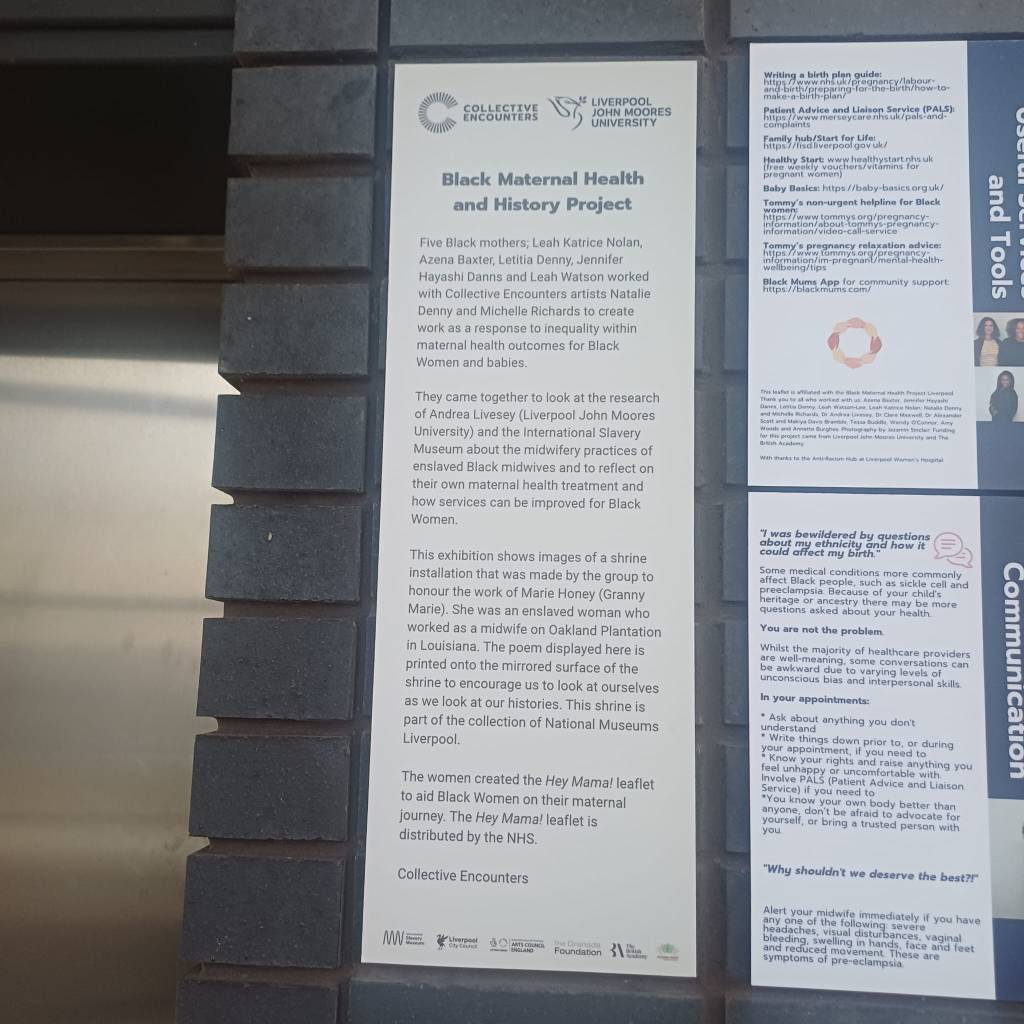
There has been excellent work done in the community about Black Maternal Health, not least the recent exhibition at Kuumba Imani Millennium Centre. Thanks to Creative Encounters for the work shown here. Photos by Teresa Williamson. There is more on this at the end of this post.
This week, a memorial, “a quiet reflective remembrance space to recognise the lives of women lost in care at the hospital”, is being opened in Liverpool Women’s Hospital. We are therefore devoting a post to this issue.
Our campaign to Save Liverpool Women’s Hospital received this message from the Hospital.
” When we last met, we discussed the development of a quiet reflective remembrance space to recognise the lives of women lost in care at the Hospital. We are delighted that this has now been completed, and we are planning to open the garden on Thursday, 6 November at 1.30 pm. There is a wider event planned with some reflective presentation from 12.30, with refreshments also in the Blair Bell, it would be lovely to see you and your other colleagues at the event.“
Outcomes in Maternity have worsened nationally, and there has been no improvement for Black and Asian women, as all services have suffered.
“Black women in England face disproportionately poor outcomes in Maternity care, shaped by systemic failings in leadership, training, data collection and accountability, according to a new report from the Health and Social Care Committee, Black Maternal Health. The inquiry heard repeatedly that racism is ‘one of the core drivers’ of poor maternal outcomes for Black women, as MPs heard from clinical experts and women about cases where racist assumptions had directly harmed Black women’s care. Black women are 2.3 times more likely to die in pregnancy, childbirth, or the postnatal period than White women, according to recent figures.
The report (from Parliament) “acknowledges that failings in care for Black women are taking place in the context of a Maternity system that is failing women more broadly, with the NHS in England having paid £27.4 billion in Maternity negligence since 2019, estimated at a figure greater than the total Maternity budget for the same period. “
The most hard-up women also suffer significantly; the women using Liverpool Women’s Hospital come from some of the most deprived areas in the UK.”Women from deprived areas of the UK are more likely than those in less deprived areas to die during or shortly after pregnancy, and this disparity has increased in recent years.“
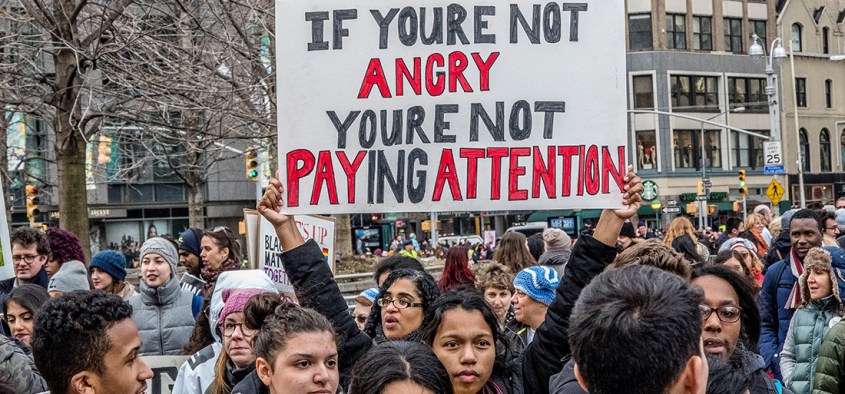
This country has disrespected birth and women’s health to such an extent that we have lost twenty years of progress. Women have had enough. Join the fightback.
Charging migrant women for Maternity care at 150% of the NHS costs is cruel, harmful, and does not recoup the costs of the system.
Asylum-seeking women can be moved around the country on the whim of the Home Office, disrupting antenatal care and costing the lives of babies and mothers.
MBBRACE-UK 2019 report “that women born outside the UK represent nearly a quarter of maternal deaths. Refugee and asylum-seeking women, despite contributing 0.29% of the population, make up 6% of this group.”
Women as a whole have seen worsening conditions.
Professor Marian Knight, Director of the National Perinatal Epidemiology Unit and MBRRACE-UK maternal reporting lead, said: “ data show that the UK maternal death rate has returned to levels that we have not seen for the past 20 years.”
Maternal deaths are not common, but still too high. Over the last century, the death rate has fallen dramatically, especially since the NHS was introduced. It is because of years of campaigning by staff and the public that maternal deaths have been reduced, but we need to do much better. The UK still has four times the maternal death rate of Norway and Denmark.
“Overall, 284 women died in 2021-23 during pregnancy or within 42 days of the end of pregnancy in the UK. The deaths of 27 women were classified as coincidental. Thus in this triennium 257 women died from direct and indirect causes, classified using ICD-MM (World Health Organisation 2012), among 2,004,184 maternities, a maternal death rate of 12.82 per 100,000 maternities (95% CI 11.30-14.49).”
In 2021, we campaigned about how babies born to Black mothers were twice as likely to suffer a stillbirth. The situation for Black mothers came into awful focus in 2024 with a terrible death at Liverpool Women’s Hospital. We wrote;
“We join with others in demanding action to make it safer for all mothers to give birth and demand action to reduce the particular risk to Black, Asian, and poor women of all races. In the UK, the rates of baby death and stillbirth among Black and Asian mothers are double those for white women. We have written about the higher number of deaths among Black babies.”
In one of these maternal deaths, investigators from the national body, Maternity and Newborn Safety Investigations (MSNI), were called in after the woman died. They reported that “The investigation into her death found hospital staff had not taken some observations because the patient was ‘being difficult'( our emphasis), according to comments in her medical notes.”…ethnicity and health inequalities impacted the care provided to the patient, suggesting that an unconscious cultural bias delayed the timing of diagnosis and response to her clinical deterioration.
Another black woman died shortly after, and we have not seen the final report, which will have been covered in the MBRRACE report this year. Such reports are confidential and focus on system issues, not on individual hospital issues.
“Each death is reviewed by assessors in four main areas: pathology, obstetrics, midwifery and anaesthetics. Where appropriate, care is also examined by speciality assessors such as psychiatrists, general practitioners and emergency medicine specialists. All reviews have a primary assessor from each speciality and, if specific issues are identified, a second assessor may also review the woman’s care.
Hospitals report each death to the Maternity and Newborn Safety Investigations programme, which reports to the families and hospitals.
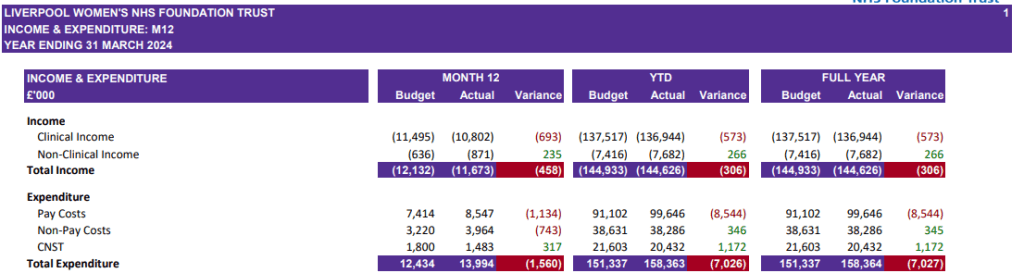
Between January 2014 and November 2023, 17 maternal deaths were recorded for patients who received care at Liverpool Women’s Hospital. We do not know the ethnic breakdown. There will have been about 70,000 births in that time, with a mortality rate of about 0.02 per cent. So deaths are quite rare.
Our campaigners were able to comment at the board meeting when the first death was announced, because the public could, at that time, attend the full board meetings of Liverpool Women’s Hospital. We knew in advance because we had read the board papers. We could then make this situation well-known. Public attendance is no longer allowed. Many times, in the early years, our campaigner, Teresa Williamson, was the only Black person in the room at these meetings, and she was not always treated with respect.
In a recent webinar about migrant women giving birth, Liverpool was highly praised for the support midwives gave to one of the speakers, who gave her experience of giving birth in total poverty. This contrasted with other women’s experiences in different parts of the country. The specialist teams at Liverpool Women’s Hospital, supporting vulnerable women in the community, do great work.
The Hospital has run a comprehensive anti-racism in service training for all staff since these deaths, together with the Anthony Walker Foundation. There is a detailed newspaper report here.
Anti-racism action, though, is like housework. It must be done again, and again, and again- even more so because there has been a rise of public racism in the politics of both the UK and the USA. This is against the decades-long trend of racism receding. Crazy ideas that Black women suffer less pain than white women are still commonly believed. One study (in the USA) found that 50% of healthcare professionals believed this. This is why anti-racism must be included in professional education.
Together with Refugee Women Connect, we met with senior members of the board of Liverpool Women’s Hospital to express our concerns. We asked for a memorial in the gardens and a pamphlet that could be reproduced in each woman’s language with illustrations, each page being available to the midwife in English to aid communication and discussion when a full translator was not available.
The memorial garden is being opened for all women who have died, and we were told that an online version of the multi-language information is being developed.
Giving birth far from home is hard for every woman. Children suffer when their mum dies. Many of the women who die in childbirth, or in the year after giving birth, would not have died had the Maternity service been appropriately staffed.
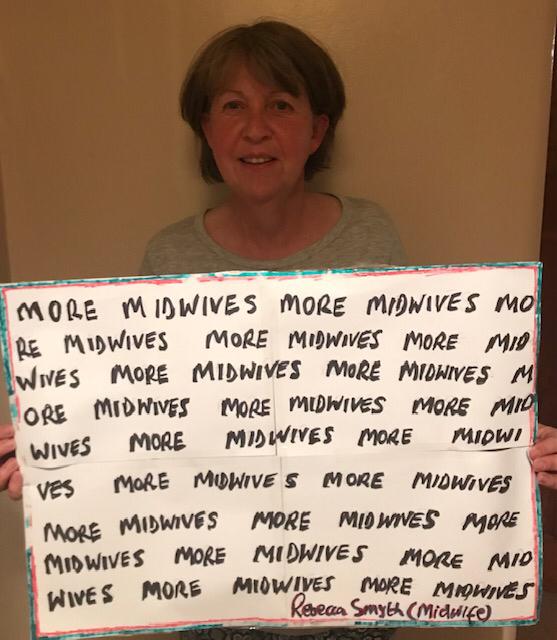
The blame for the state of Maternity lies squarely with the politicians. They have made the decisions on funding and staffing. They brought in austerity. Midwives are overworked. Obstetricians are overworked, as are other linked professionals and the ancillary staff. They are too overworked to give the quality of healthcare women need. This harms midwives and mothers. Staff need time to think, reflect, and discuss. We will continue to demand fundamental improvements in funding, staffing, and NHS management.
Maternity staff carry huge responsibilities and deliver an excellent service when they can, but no one can be perfect when there are too few staff and poor organisation. Neither can they be expected to fight for improvements alone. The public must take a major part.
The management systems of the NHS (especially since 2012, and then 2022, with the appalling Health and Care Acts that treated the NHS as a business, not a public service) have made staff feel they cannot raise concerns or that those concerns will be ignored. This has been reflected in many of the Maternity enquiries, including the Kirkup enquiry into the Maternity tragedies in Morecombe Bay.
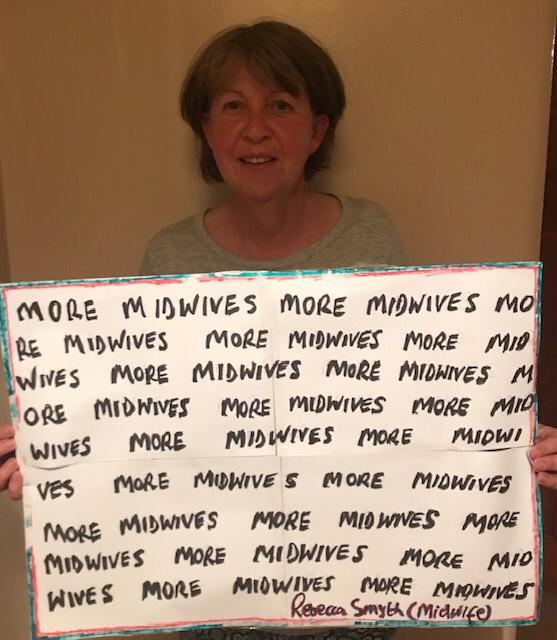
This country can and must afford a good Maternity service; we currently rank 17th out of 19 wealthy countries for the safety of our Maternity services. In the first twenty years of this century, everywhere but the UK and the USA improved their Maternity care. We need more midwives. We need more midwives.
Please keep fighting for all our mothers, sisters, daughters, friends, lovers, and every precious baby.